 The adrenal glands are the main stress control system of the body. Adrenal Fatigue is a decrease in the adrenal glands’ ability to carry out this normal function. It is commonly caused by chronic stress from any source (including emotional, physical, mental, or environmental) that exceeds the body’s capacity to adjust appropriately to the demands placed on it by the stress. Stressors that can lead to Adrenal Fatigue include anger, chronic illness, depression, surgery, high sugar intake, over exercise, sleep deprivation, chronic or acute infections including Giardia and H. pylori and root canal repair, just to mention a few.
The adrenal glands are the main stress control system of the body. Adrenal Fatigue is a decrease in the adrenal glands’ ability to carry out this normal function. It is commonly caused by chronic stress from any source (including emotional, physical, mental, or environmental) that exceeds the body’s capacity to adjust appropriately to the demands placed on it by the stress. Stressors that can lead to Adrenal Fatigue include anger, chronic illness, depression, surgery, high sugar intake, over exercise, sleep deprivation, chronic or acute infections including Giardia and H. pylori and root canal repair, just to mention a few.
Signs and symptoms of Adrenal Fatigue include tendency to gain weight and inability to lose it, especially around the waist, high frequency of getting the flu and other respiratory diseases with symptoms that tend to last longer than usual, tendency to tremble when under pressure, reduced sex drive, lightheadedness when rising from a prone position, brain fog, lack of energy in the afternoon, reliance on coffee to get the day started, fibromyalgia, chronic fatigue, craving for salty and fatty foods, hypoglycemia, chronic pain of unknown origin and feeling better during a vacation. None of these signs or symptoms by themselves can definitively point to Adrenal Fatigue. However, as a group of symptoms, in the context of an otherwise healthy person, they do form a specific Adrenal Fatigue Syndrome or picture, that is, of a person under stress and the body’s failing physiological response to deal with such a burden. Adrenal Fatigue, as a debilitating condition, is not recognized by conventional medicine and is thus missed by most conventionally trained physicians.
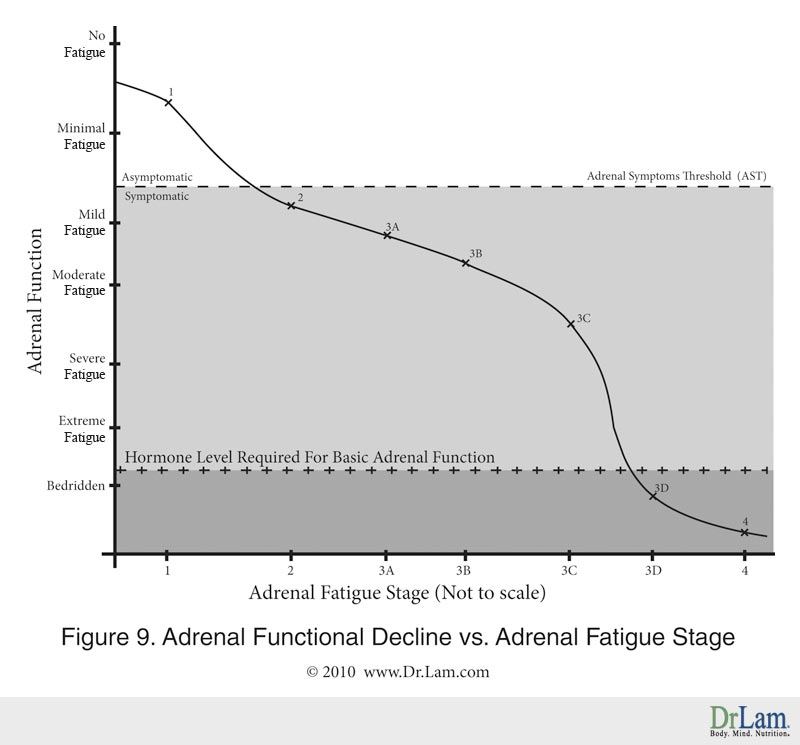
Adrenal Fatigue progresses through four advancing stages with increased severity of symptoms with each stage as illustrated below:

In this stage, the body is alarmed by the stressors and mounts an aggressive anti-stress response to overcome the stressors. This anti-stress response is mediated by an increase in anti-stress hormones like cortisol. The amount of anti-stress hormone required is well within the body’s output capacity. Fatigue is usually quite mild and usually occurs in the morning upon awakening or in the mid-afternoon. No physical or physiological dysfunction is clinically noticeable. Normal daily function is expected, though peak performance cannot be achieved. Adrenal crash may have occurred but normally it is undetectable.
The adrenal glands are usually the first in order of endocrine function to breakdown in a stressful situation that has overwhelmed the body’s normal compensatory response. Unfortunately, Adrenal Fatigue is a sub-clinical state that is seldom recognized as a pathological condition. Acceptable social compensatory actions such as coffee intake often mask the underlying problem: the adrenals are put into over-drive to cover up the early signs and symptoms of fatigue. The insulin-producing portion of the pancreas is also affected. Imbalance in blood sugar level results in low energy and this dysfunction is temporarily fixed by quick fixes such as high sugar content soda drinks, energy potions and high carbohydrate foods such as donuts. Many people even consider this state “normal” as part of living in the modern society. Those who require coffee to “kick start” the day may already suffer from Adrenal Fatigue without being aware of it.

With chronic or severe stress, the adrenals are eventually unable to keep up with the body’s demand for cortisol. Adrenal Fatigue now enters into Stage 2. Normal daily functions can still be carried out, but the sense of fatigue is pronounced at the end of each day as the body needs more rest than usual to recover.Despite a full night’s rest, the body does not feel refreshed in the morning. Anxiety starts to set in and the person becomes easily irritable. Insomnia becomes more common, as it takes longer to fall asleep and there are frequent awakenings as well. Infections become recurrent. PMS and menstrual irregularities surface and symptoms suggestive of hypothyroidism (such as a sensation of feeling cold and a sluggish metabolism) become prevalent. The thyroid glands are usually affected at this stage. Sluggishness, feeling cold, and weight gain centrally, despite exercise and diet, are the predominant symptoms that usually bring the patients to their physicians for the first time. Thyroid replacement is routinely prescribed but ovarian hormones, synthetic or bio-identical, are also considered. However, the vast majority of patients who undergo such hormonal adjustment remain symptomatic over time and their treatments usually fail. Many people will visit their physicians for the first time at this stage. Conventional medical work up is ordered, but the test results are inevitably within range and patients are sent home with no concrete program for recovery. At this stage, many people are prescribed anti-depressants. The many warning signs of the body continue to be ignored, as most people will rely on more and more stimulants to keep their mood up. Those who require multiple cups of coffee to sustain them may well be entrenched at this stage without knowing it. Conventional medicine, unfortunately, does not recognize Adrenal Fatigue as a medical condition. Typically, symptoms are treated and not the root cause of the problem.
Adrenal Exhaustion refers to Stage 3 of Adrenal Fatigue. As adrenal function is weakened further, the body’s need for adrenal hormones remains unabated if stress is not reduced. The adrenals are no longer able to keep up with the ever-increasing demand for cortisol production needed to overcome the stress and they become exhausted. Cortisol output starts to decline and this usually happens gradually. If the stressors are severe, an adrenal crash may occur, to be followed by a longer than usual recovery. The body, at this stage of Adrenal Fatigue, has, as its primary goal, the conservation of energy to ensure survival. Systematically, the body goes into a slow-down mode and starts to break down muscle tissue to produce energy. This catabolic stage results in the breakdown of muscles and protein wasting. Chronic fatigue is common and exercise tolerance is reduced. Concurrently, chronic fibromyalgia appears. Toxic metabolites begin to accumulate throughout the body, leading to brain fog and insomnia. Depression becomes severe and constant. As this stage progresses, metabolic, immunological and neurological single organ systems dysfunction characteristic of Stage 2 Adrenal Fatigue becomes chronic (Phase A). It then spreads to involve multiple organs (Phase B). This is evidenced by multiple endocrine axis dysfunctions, including the ovarian-adrenal-thyroid axis imbalance in females and adrenal-thyroid axis imbalance in males.
 If not attended to, the body is further weakened and enters into a state of disequilibrium with loss of homeostasis (Phase C). As the body tries to repair itself with the limited tools it has, there are wild, exaggerated and paradoxical autonomic-driven reactions. These are characterized by adrenaline rushes, labile blood pressure, and hypoglycemic episodes after meals and anxiety attacks. A state of near adrenal failure (Phase D) eventually occurs as the body’s pool of hormones reaches a level too low to prime the adrenals. Without sufficient levels of hormones, the body goes into a full-blown shut down mode to stop as much of the non-essential functions as possible to conserve energy in order to survive. During this stage of Adrenal Fatigue, the libido is suppressed, digestion slows down and metabolic rate declines to conserve body weight. Those afflicted find themselves bed-ridden most of the time, and have energy that will last for only a short time.
If not attended to, the body is further weakened and enters into a state of disequilibrium with loss of homeostasis (Phase C). As the body tries to repair itself with the limited tools it has, there are wild, exaggerated and paradoxical autonomic-driven reactions. These are characterized by adrenaline rushes, labile blood pressure, and hypoglycemic episodes after meals and anxiety attacks. A state of near adrenal failure (Phase D) eventually occurs as the body’s pool of hormones reaches a level too low to prime the adrenals. Without sufficient levels of hormones, the body goes into a full-blown shut down mode to stop as much of the non-essential functions as possible to conserve energy in order to survive. During this stage of Adrenal Fatigue, the libido is suppressed, digestion slows down and metabolic rate declines to conserve body weight. Those afflicted find themselves bed-ridden most of the time, and have energy that will last for only a short time.
What separates Stage 3 Adrenal Fatigue from earlier stages, clinically, is that the patient often cannot function smoothly throughout the day, no matter how hard he tries. The adrenal function is constantly hovering around the adrenal symptoms threshold level and the smallest stressor will often trigger an adrenal crash. Not only is recovery time taking longer but the body never fully returns to the pre-crash baseline energy level. Something is wrong and the body’s cry for help becomes louder. The productive hours of the day will progressively decrease and it is not unusual for those at this stage of Adrenal Fatigue to have only a few hours of productive time a day, while the rest of the time is spent in bed resting.
Eventually, the adrenals will become totally exhausted. Patients at this stage will have a high chance of cardiovascular collapse and death. When Adrenal Fatigue has advanced to this stage, the line between it and Addison’s disease, also called adrenal insufficiency, can be blurred. While the etiology of the two conditions may be different, the ultimate clinical presentations can be quite similar as they both represent a continuum of decompensation in adrenal function. When Adrenal Fatigue reaches this stage, the severe advanced adrenal crisis manifestation can be very similar and akin to an Addisonian crisis or acute adrenal insufficiency which, is a recognized medical condition. Symptoms of this include sudden, penetrating pain in the lower back, abdomen or legs, severe vomiting and diarrhea, dehydration, low blood pressure and loss of consciousness. Addisonian crisis is rare and in most cases, the symptoms are severe enough that patients often seek medical treatment before a crisis occurs. However, in about 25 percent of patients, the symptoms first appear during an Addisonian crisis. If left untreated, the Addisonian crisis can be fatal.
Although adrenal dysfunction and its various stages were recognized as distinct clinical syndromes since the turn of the 20th century, most conventionally trained physicians are still unfamiliar with this condition because it is difficult to diagnose through traditional blood tests. Most patients are sent home with anti-depressants after a short trial of hormonal replacement but this will usually fail.
 Depletion and dysregulation of adrenal hormones such as cortisol and adrenaline are the primary symptomatic drivers of Adrenal Fatigue and crashes. Repeated crashes over time will invariably further weaken the adrenal glands. While the intensity of each crash will increase as Adrenal Fatigue increases, it is not a linear progression clinically. Many in Stage 1 and Stage 2 Adrenal Fatigue are not aware of their impending problems. Their daily activities will remain unchanged, as there is sufficient adrenal reserve to compensate for any transient energy low.
Depletion and dysregulation of adrenal hormones such as cortisol and adrenaline are the primary symptomatic drivers of Adrenal Fatigue and crashes. Repeated crashes over time will invariably further weaken the adrenal glands. While the intensity of each crash will increase as Adrenal Fatigue increases, it is not a linear progression clinically. Many in Stage 1 and Stage 2 Adrenal Fatigue are not aware of their impending problems. Their daily activities will remain unchanged, as there is sufficient adrenal reserve to compensate for any transient energy low.
Many in Adrenal Fatigue Stage 3A and Stage 3B continue to hold their full time jobs. Extra rest is usually needed, but those with strong body constitutions can make it through for years. Decline in adrenal function is slow and steady and sometimes this is written off as the effect of aging.
For most, Adrenal Fatigue Stage 3C is a wake up call as moderate fatigue may become severe. The decline can be fast and furious and an adrenal crash can occur in a matter of hours. One can be bedridden for days, with slow recovery. Those who are constitutionally weak will have the most difficult time recovering. The decline in adrenal function is most rapid in this phase. The body’s energy level comes crashing down like a waterfall. This “slow down” mode is new to most people whose lives have been active before and this is most unpleasant.
Interestingly, functional decline actually slows down in Stage 3D as compared to Stage 3C. There is already an extremely low level of hormones remaining and the body is rapidly down-regulating to stop most non-essential bodily functions to ensure survival. The body is in a “shut down” mode and is trying to get used to the low energy state. Most people will be bedridden at this stage requiring ambulatory help.
Any small stressor may trigger a drop below the level required for minimum basic adrenal function and this may in turn trigger adrenal failure, as shown in the following graphic representation. The above is summarized in the following graph:
While Stage 1 (flight or fight response) and Stage 2 (organ resistance) of Adrenal Fatigue have been studied from a patho-physiological perspective for some decades, our clinical understanding of the myriad of symptoms and their convoluted presentations in Stage 3 (Adrenal Exhaustion) is still in its infancy at best.
Stage 3 (Adrenal Exhaustion) Adrenal Fatigue is the most complicated because in this stage the body’s multiple organ systems become systematically decompensated concurrently.
Because the variety of symptoms presented at this stage can be convoluted and overwhelming, it is helpful, from a clinical perspective, to further delineate this stage into four broad overlapping phases. The boundaries of each phase are decidedly indistinct, and they represent the body’s strategy of returning to a simple physiological state where energy is conserved. The different phases of Adrenal Fatigue do not represent an absolute sequential gradation process and should not be viewed as such. Laboratory tests remain unremarkable, while symptoms become more pronounced. Most people, if not all, who are suffering from Adrenal Exhaustion usually present their signs and symptoms in various degrees in each phase concurrently. That is the norm and more advanced cases of Adrenal Exhaustion presents the later phase of manifestation.
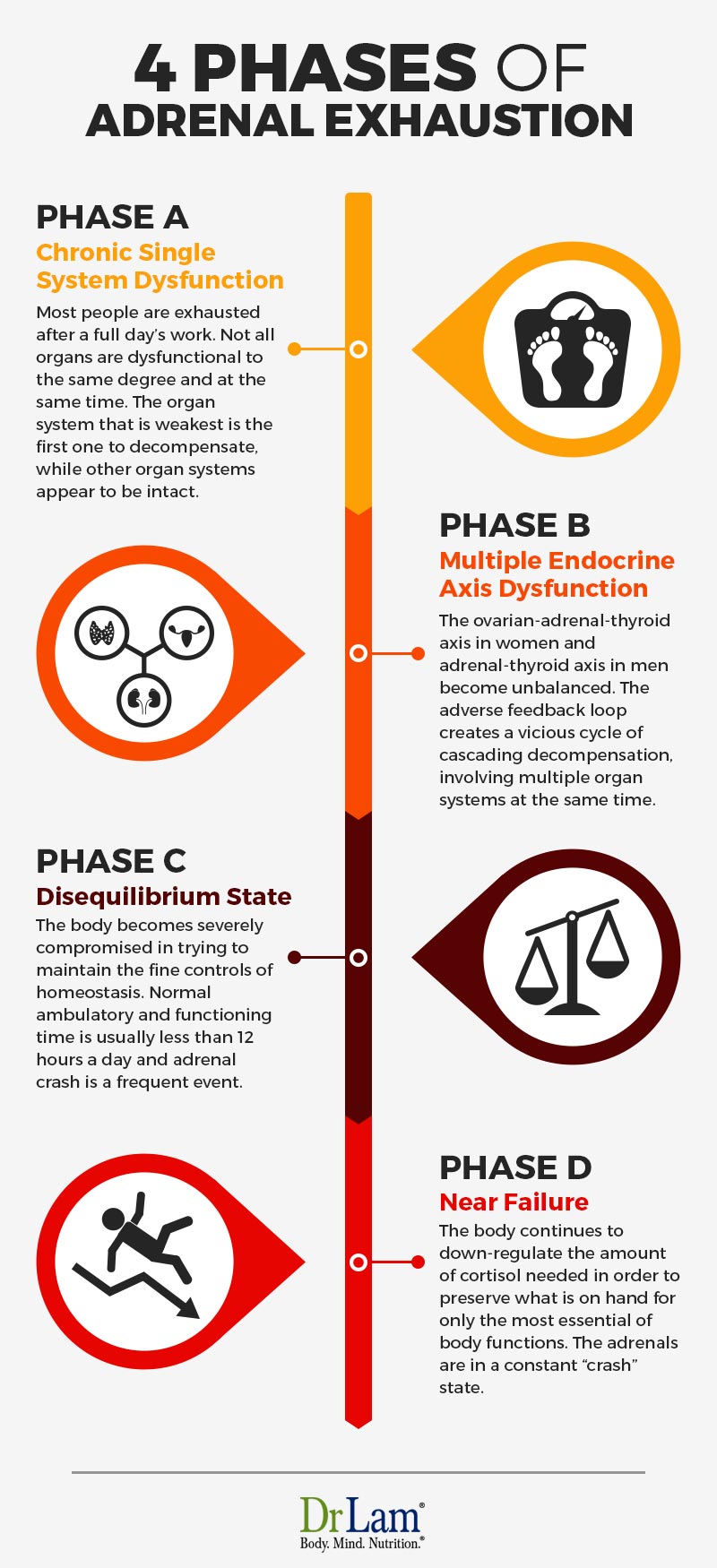
 In this phase, mild symptoms characteristic of Stage 1 and Stage 2 Adrenal Fatigue continue to worsen and become persistent or chronic. A few symptoms that are commonly found during these two phases of Adrenal Fatigue are slightly elevated blood pressure that becomes low throughout the day, mild musculoskeletal pain that turns into chronic fibromyalgia around the clock, frequent recurrent infections become the norm as opposed to intermittent infections, occasional feelings of the “blues” becomes mild depression, sleep patterns become more disrupted as insomnia becomes chronic, and fatigue that usually occurs during the end of occasional stressful days becomes an everyday event. There is moderate reduction in carrying out normal daily activities. Most people are exhausted after a full day’s work. Not all organs are dysfunctional to the same degree and at the same time. The organ system that is constitutionally weakest is the first one to decompensate, while other organ systems appear to be intact. For example, one may have severe insomnia, but otherwise feel all right, relatively speaking. Those who are metabolically weak may start to notice significant weight gain, especially in the center part of the body, accompanied by difficulty in losing the weight despite doing vigorous exercise. These are all classic symptoms of Adrenal Fatigue. Sufferers at this time usually recognize that something is wrong and most of them have already been evaluated by their physicians but continue to be active physically with some difficulty. Many will search the Internet for more information and possibly embarked on self-guided programs or see their health professionals. Numerous doctors may have been consulted at this time, while the patient’s condition does not usually improve over time, but in fact, becomes worse.
In this phase, mild symptoms characteristic of Stage 1 and Stage 2 Adrenal Fatigue continue to worsen and become persistent or chronic. A few symptoms that are commonly found during these two phases of Adrenal Fatigue are slightly elevated blood pressure that becomes low throughout the day, mild musculoskeletal pain that turns into chronic fibromyalgia around the clock, frequent recurrent infections become the norm as opposed to intermittent infections, occasional feelings of the “blues” becomes mild depression, sleep patterns become more disrupted as insomnia becomes chronic, and fatigue that usually occurs during the end of occasional stressful days becomes an everyday event. There is moderate reduction in carrying out normal daily activities. Most people are exhausted after a full day’s work. Not all organs are dysfunctional to the same degree and at the same time. The organ system that is constitutionally weakest is the first one to decompensate, while other organ systems appear to be intact. For example, one may have severe insomnia, but otherwise feel all right, relatively speaking. Those who are metabolically weak may start to notice significant weight gain, especially in the center part of the body, accompanied by difficulty in losing the weight despite doing vigorous exercise. These are all classic symptoms of Adrenal Fatigue. Sufferers at this time usually recognize that something is wrong and most of them have already been evaluated by their physicians but continue to be active physically with some difficulty. Many will search the Internet for more information and possibly embarked on self-guided programs or see their health professionals. Numerous doctors may have been consulted at this time, while the patient’s condition does not usually improve over time, but in fact, becomes worse.
The endocrine system in our body is linked hormonally in a series of axes for optimal function. Dysfunction in one system invariably affects the others, leading to a cascade of decompensation as the body weakens and Adrenal Fatigue moves on to the next phase. The ovarian-adrenal-thyroid axis in women and adrenal-thyroid axis in men are particularly important as they relate to adrenal function. When these axis become unbalanced, the adverse feedback loop creates a vicious cycle of cascading decompensation, involving multiple organ systems at the same time. Imbalance of these axes is the hallmark in Phase B. Typical presentations in females involve symptoms of under-active thyroid, unbalanced ovarian hormones, and low adrenal function. In males, the adrenal-thyroid axis may be compromised. The sufferer’s physical and emotional states continue to deteriorate and he enters into a state of confusion in this phase of Adrenal Fatigue, as he is unable to logically dissect the myriad of systematic manifestations of multiple hormonal axis imbalances. Almost all conventionally trained and many naturally oriented physicians alike are at a loss. Patients are often abandoned to self-navigate through these turbulent waters. Not knowing what to do and who to turn to, sufferers of Adrenal Fatigue will self-navigate, often using inappropriate nutrients that are not conducive to healing while subjecting their bodies to continued trial and error. This often worsens the condition over time.
 As the body continues its downward path of impaired functions, it gathers steam. Gradually, the body becomes severely compromised in trying to maintain the fine controls of homeostasis. Normal equilibrium is therefore lost. The body will try its hardest to maintain equilibrium but its crude compensatory response, damaged receptor sites, along with impaired metabolic and detoxification pathways, give rise to paradoxical and exaggerated responses. This is usually mediated through the autonomic nervous system. The body’s internal thermostat is now “broken” and normal regulation is severely compromised. The body activates its reserve system to maintain homeostasis but unfortunately, the body’s reserve system lacks the fine control of regular systems. The body’s crude and exaggerated responses will further weaken the existing compromised adrenal function while further negatively affecting your Adrenal Fatigue state. Clinical manifestation includes swings in blood sugar levels with reactive hypoglycemia being the hallmark, fragile blood pressure state, postural hypotension, inability to remain standing for a prolonged period of time, reactive hyper-adrenergic responses including heart palpitations, night sweats, and a state of reactively driven anxiety followed by depression. The body is literally running on its “spare tires” to survive, and “falling apart” internally. Sufferers at this phase of Adrenal Fatigue will often become incapacitated and are frequently called the “living dead.” Normal ambulatory and functioning time is usually less than 12 hours a day and adrenal crash is a frequent event. It is imperative that care at this time be totally turned over to a qualified specialist, as this level of dysfunction is well beyond the expertise of even the most astute naturally oriented health care provider.
As the body continues its downward path of impaired functions, it gathers steam. Gradually, the body becomes severely compromised in trying to maintain the fine controls of homeostasis. Normal equilibrium is therefore lost. The body will try its hardest to maintain equilibrium but its crude compensatory response, damaged receptor sites, along with impaired metabolic and detoxification pathways, give rise to paradoxical and exaggerated responses. This is usually mediated through the autonomic nervous system. The body’s internal thermostat is now “broken” and normal regulation is severely compromised. The body activates its reserve system to maintain homeostasis but unfortunately, the body’s reserve system lacks the fine control of regular systems. The body’s crude and exaggerated responses will further weaken the existing compromised adrenal function while further negatively affecting your Adrenal Fatigue state. Clinical manifestation includes swings in blood sugar levels with reactive hypoglycemia being the hallmark, fragile blood pressure state, postural hypotension, inability to remain standing for a prolonged period of time, reactive hyper-adrenergic responses including heart palpitations, night sweats, and a state of reactively driven anxiety followed by depression. The body is literally running on its “spare tires” to survive, and “falling apart” internally. Sufferers at this phase of Adrenal Fatigue will often become incapacitated and are frequently called the “living dead.” Normal ambulatory and functioning time is usually less than 12 hours a day and adrenal crash is a frequent event. It is imperative that care at this time be totally turned over to a qualified specialist, as this level of dysfunction is well beyond the expertise of even the most astute naturally oriented health care provider.
As the body’s cortisol hormone level falls below the minimum level required for normal functions and cortisol output fails during this stage of Adrenal Fatigue, the body continues to down-regulate the amount of cortisol needed in order to preserve what is on hand for only the most essential of body functions. The adrenals are in a constant “crash” state. Pump-failure occurs. This down-regulation further reduces cortisol output thereby exaggerating a vicious downward cycle. Toleration to steroids may be blunted or negative. Normal nutrients are often systemically rejected by the body, even at low doses. This stage of Adrenal Fatigue is not to be self-navigating and expert professional guidance is essential at this time. Unfortunately, qualified physicians in this area are extremely a state rare. Normal ambulatory and functioning time is usually under six to eight hours a day.
Let us now do an in-depth examination of each of these phases of Adrenal Fatigue.
A weak adrenal system and its accompanying Adrenal Fatigue will bring about profound systemic decompensatory actions and reactions, manifesting in a wide range of symptoms. In this phase, one or more of the body systems has weakened to such a point that a pathological clinical state of the affected system surfaces. The organs affected can be broadly classified into five major categories:
 Hypoglycemia (low blood sugar) is common in Adrenal Exhaustion and this is usually due to the combination of low cortisol and high insulin levels when the body is under stress. The normal stress response, by the adrenals, is to increase the blood glucose level by increasing the cortisol output. This is commonly seen in Stage 1 and 2 of Adrenal Fatigue. As the output of cortisol is reduced in Adrenal Exhaustion (Stage 3), discharge of glucose is slowed and the blood sugar level tends to fall. At the same time, insulin modulation becomes more dysregulated at this stage due to irregular and unstable blood sugar levels associated with metabolic syndrome if it is present. The release of insulin from the pancreas tends to be over-reactive at times and is thus high in such a condition. The combination of low cortisol, as is typically common during this particular stage of Adrenal Fatigue, along with a high insulin level, leads to hypoglycemia and common symptoms of low blood sugar include dizziness and fainting. As cellular energy demand is not being met by a sufficient level of blood glucose, the body will turn to proteins and fats as the source of energy. This pathway is not as efficient; but is nevertheless put on overdrive in order to provide the much needed energy. Without adequate cortisol levels to elevate the blood sugar levels by facilitating the conversion of glycogen, fats, and proteins to new glucose supplies, this increased demand is difficult to meet. Clinically, one of the hallmarks of Adrenal Exhaustion is irregular blood sugar patterns with hypoglycemia. People with Adrenal Exhaustion often find themselves in a no-win situation. When people are under stress (even a mild stress such as a mild argument or excessive homework), the demand for blood glucose increases, but their exhausted adrenals cannot produce enough cortisol to generate higher glucose levels from the body’s reserves. In the presence of increased insulin and decreased cortisol, the blood sugar level will drop off rapidly.Hypoglycemia itself is a significant stress on the entire body, and especially on the adrenals. While this can be overcome with a “sugar fix “consisting of an instant load of sugary drink or foods such as coffee or soda, this is a short term emergency remedy only. Usually the symptoms will go away immediately, but then return after one to two hours. Reactivation and restoration of normal cell function requires extra amounts of energy beyond the requirements for normal maintenance. With each hypoglycemic episode, more cells are damaged. Thus, the body reaches a new low with each recurrence of hypoglycemia. If this happens at the same time as the body faces an increasing demand for glucose, the stage is set for an adrenal crisis. With each plunge, Adrenal Fatigue increases and hypoglycemia worsens. By the end of the day, the person may feel nearly exhausted without having done anything productive. Low blood sugar levels are most likely to occur around 10:00 AM, 2:00 PM and from 3 – 4:00 PM. If not reversed, it often progresses to adult onset diabetes as well. Diabetes, especially type-2 diabetes, more often than not, is the direct result of prolonged Adrenal Fatigue.
Hypoglycemia (low blood sugar) is common in Adrenal Exhaustion and this is usually due to the combination of low cortisol and high insulin levels when the body is under stress. The normal stress response, by the adrenals, is to increase the blood glucose level by increasing the cortisol output. This is commonly seen in Stage 1 and 2 of Adrenal Fatigue. As the output of cortisol is reduced in Adrenal Exhaustion (Stage 3), discharge of glucose is slowed and the blood sugar level tends to fall. At the same time, insulin modulation becomes more dysregulated at this stage due to irregular and unstable blood sugar levels associated with metabolic syndrome if it is present. The release of insulin from the pancreas tends to be over-reactive at times and is thus high in such a condition. The combination of low cortisol, as is typically common during this particular stage of Adrenal Fatigue, along with a high insulin level, leads to hypoglycemia and common symptoms of low blood sugar include dizziness and fainting. As cellular energy demand is not being met by a sufficient level of blood glucose, the body will turn to proteins and fats as the source of energy. This pathway is not as efficient; but is nevertheless put on overdrive in order to provide the much needed energy. Without adequate cortisol levels to elevate the blood sugar levels by facilitating the conversion of glycogen, fats, and proteins to new glucose supplies, this increased demand is difficult to meet. Clinically, one of the hallmarks of Adrenal Exhaustion is irregular blood sugar patterns with hypoglycemia. People with Adrenal Exhaustion often find themselves in a no-win situation. When people are under stress (even a mild stress such as a mild argument or excessive homework), the demand for blood glucose increases, but their exhausted adrenals cannot produce enough cortisol to generate higher glucose levels from the body’s reserves. In the presence of increased insulin and decreased cortisol, the blood sugar level will drop off rapidly.Hypoglycemia itself is a significant stress on the entire body, and especially on the adrenals. While this can be overcome with a “sugar fix “consisting of an instant load of sugary drink or foods such as coffee or soda, this is a short term emergency remedy only. Usually the symptoms will go away immediately, but then return after one to two hours. Reactivation and restoration of normal cell function requires extra amounts of energy beyond the requirements for normal maintenance. With each hypoglycemic episode, more cells are damaged. Thus, the body reaches a new low with each recurrence of hypoglycemia. If this happens at the same time as the body faces an increasing demand for glucose, the stage is set for an adrenal crisis. With each plunge, Adrenal Fatigue increases and hypoglycemia worsens. By the end of the day, the person may feel nearly exhausted without having done anything productive. Low blood sugar levels are most likely to occur around 10:00 AM, 2:00 PM and from 3 – 4:00 PM. If not reversed, it often progresses to adult onset diabetes as well. Diabetes, especially type-2 diabetes, more often than not, is the direct result of prolonged Adrenal Fatigue. Detoxification dysfunction leading to a low-clearance state. Nutrients needed by the body usually come from foods or natural compounds, such as vitamins. In this phase of Adrenal Exhaustion, the body’s ability to process and excrete waste by-products after nutrients have been assimilated by the cells is invariably compromised due to the low energy state. As the body slows down, so does the body’s digestive, absorptive and excretion mechanisms. Normal body function requires optimum and timely processing of nutrients by the liver once they are ingested and absorbed in the gut. Unwanted waste by-products and metabolites are subsequently excreted out of the body through the kidneys, lungs, skin, and gastrointestinal tract. Without proper and timely clearance, the body may slowly accumulate undesirable waste by-products or metabolites internally. Instead of being excreted out of the body, they remain in circulation. The more advanced the Adrenal Fatigue, the more serious this problem becomes. Without proper detoxification and clearance out of the body, unwanted metabolites accumulate and become toxic inside the body. This negatively impacts Adrenal Fatigue and compounds the symptoms of the condition.Proper clearance of metabolites and toxins is thus a major concern. The liver is the major detoxification center of the body. It acts as an “in-line” filter for the removal of foreign substances and wastes from the blood. Toxins cleared by the liver include alcohol, solvents, formaldehyde, pesticides, herbicides and food additives. Despite varying chemical toxicity, the liver has the function of reducing toxins into compounds that the body can safely handle and remove through the kidneys (as urine), skin (as sweat), lungs (as expelled air) and bowels (as feces). Optimal liver function is therefore essential for good health. The liver is also responsible for breaking down nutrients, vitamins, and hormones into small inert metabolites once their usefulness has been served. These metabolites are then excreted. The slowing down of the detoxification process, seen in Adrenal Fatigue, can lead to a low-clearance state, with the accumulation of unwanted metabolites which can then turn toxic inside the body.Circulating metabolites may find themselves a home in the extracellular spaces of joints, causing joint pain of unknown origin. Many such metabolites are fat-soluble and they cross the blood-brain barrier into the brain and tend to accumulate there, resulting in brain-fog, anxiety and insomnia. Some are deposited into the muscles, contributing to chronic fatigue and muscle pain. Other symptoms include psychological and neurological symptoms such as depression, headache, mental confusion, mental illness, abnormal nerve reflexes and tingling in the hands. These are all common symptoms of adrenal failure and the accompanying Adrenal Fatigue that sets in.This low clearance state usually starts to exhibit itself in this phase, but tends to get much worse as Adrenal Exhaustion progresses.
Detoxification dysfunction leading to a low-clearance state. Nutrients needed by the body usually come from foods or natural compounds, such as vitamins. In this phase of Adrenal Exhaustion, the body’s ability to process and excrete waste by-products after nutrients have been assimilated by the cells is invariably compromised due to the low energy state. As the body slows down, so does the body’s digestive, absorptive and excretion mechanisms. Normal body function requires optimum and timely processing of nutrients by the liver once they are ingested and absorbed in the gut. Unwanted waste by-products and metabolites are subsequently excreted out of the body through the kidneys, lungs, skin, and gastrointestinal tract. Without proper and timely clearance, the body may slowly accumulate undesirable waste by-products or metabolites internally. Instead of being excreted out of the body, they remain in circulation. The more advanced the Adrenal Fatigue, the more serious this problem becomes. Without proper detoxification and clearance out of the body, unwanted metabolites accumulate and become toxic inside the body. This negatively impacts Adrenal Fatigue and compounds the symptoms of the condition.Proper clearance of metabolites and toxins is thus a major concern. The liver is the major detoxification center of the body. It acts as an “in-line” filter for the removal of foreign substances and wastes from the blood. Toxins cleared by the liver include alcohol, solvents, formaldehyde, pesticides, herbicides and food additives. Despite varying chemical toxicity, the liver has the function of reducing toxins into compounds that the body can safely handle and remove through the kidneys (as urine), skin (as sweat), lungs (as expelled air) and bowels (as feces). Optimal liver function is therefore essential for good health. The liver is also responsible for breaking down nutrients, vitamins, and hormones into small inert metabolites once their usefulness has been served. These metabolites are then excreted. The slowing down of the detoxification process, seen in Adrenal Fatigue, can lead to a low-clearance state, with the accumulation of unwanted metabolites which can then turn toxic inside the body.Circulating metabolites may find themselves a home in the extracellular spaces of joints, causing joint pain of unknown origin. Many such metabolites are fat-soluble and they cross the blood-brain barrier into the brain and tend to accumulate there, resulting in brain-fog, anxiety and insomnia. Some are deposited into the muscles, contributing to chronic fatigue and muscle pain. Other symptoms include psychological and neurological symptoms such as depression, headache, mental confusion, mental illness, abnormal nerve reflexes and tingling in the hands. These are all common symptoms of adrenal failure and the accompanying Adrenal Fatigue that sets in.This low clearance state usually starts to exhibit itself in this phase, but tends to get much worse as Adrenal Exhaustion progresses. It comes as no surprise that people in this phase of Adrenal Fatigue complain of an increase in unclear thinking, difficulty in concentrating, anxiety, food allergies, multiple chemical sensitivity, food intolerance (especially dairy, wheat, and corn products, all of which are hard to digest), pain of unknown origin, insomnia, anxiety, food coma, increase in the incidence of yeast infection, candidiasis, irritable bowel, chronic fatigue and interstitial cystitis among others. These are warning signs of the body’s low-clearance state.Gradual intolerance of previously acceptable compounds or environmental settings is a warning sign that the body is now entering into a low-clearance state. This intolerance can include vitamins, minerals, glandular, herbs, medications, food, chemical sensitivity, electro-magnetic waves, fluorescent lighting, and computer monitor screens, just to name a few.
It comes as no surprise that people in this phase of Adrenal Fatigue complain of an increase in unclear thinking, difficulty in concentrating, anxiety, food allergies, multiple chemical sensitivity, food intolerance (especially dairy, wheat, and corn products, all of which are hard to digest), pain of unknown origin, insomnia, anxiety, food coma, increase in the incidence of yeast infection, candidiasis, irritable bowel, chronic fatigue and interstitial cystitis among others. These are warning signs of the body’s low-clearance state.Gradual intolerance of previously acceptable compounds or environmental settings is a warning sign that the body is now entering into a low-clearance state. This intolerance can include vitamins, minerals, glandular, herbs, medications, food, chemical sensitivity, electro-magnetic waves, fluorescent lighting, and computer monitor screens, just to name a few.
Fortunately, this low-clearance state can often be reversed once adrenal health is normalized. The danger lies in not recognizing the symptoms as signs of the body’s underlying low-clearance state. The tendency is to treat the symptoms, especially by those trying to self-navigate. Many will embark on various aggressive detoxification programs in their efforts to combat Adrenal Fatigue, only to end up worse off, due to retoxification reactions. Treating the symptoms of Adrenal Fatigue will mask the body’s underlying low clearance state. Without proper intervention and reversal, this low-clearance state tends to progressively get worse as Adrenal Exhaustion advances.
While the mild to moderate low-clearance state is a characteristic of Phase A Adrenal Exhaustion, a severe low-clearance state is a hallmark of Phase D Adrenal Exhaustion and we will examine that in greater detail later.
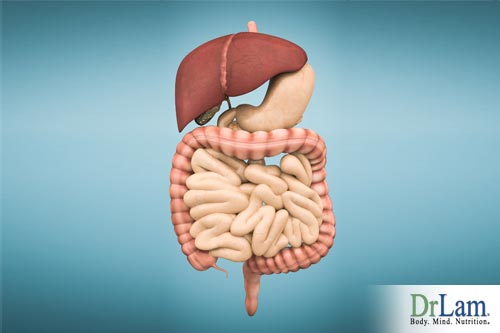 As the collagen structure of internal organs break down, their functions are compromised. For example, gastrointestinal track motility and contraction forces are reduced. Adrenal Exhaustion is often associated with a poor ability to digest proteins. Common symptoms during this phase of Adrenal Fatigue include constipation, indigestion and irritable bowel syndrome. The amount of acid production may not be sufficient to help break down foods, resulting in further improper digestion and assimilation of nutrients. At the ortho-molecular level, cells are deprived of the much needed nutrients despite a healthy diet with balanced macro-nutritional factors.It is no surprise that secondary fibromyalgia and chronic fatigue syndrome are commonly associated with Adrenal Exhaustion. Many have postulated that Adrenal Fatigue often precedes fibromyalgia and chronic fatigue. There is no doubt, clinically, that Adrenal Exhaustion contributes to the overall fibromyalgia chronic fatigue picture, no matter what the cause. Proteins are made up of amino acids. Just as sugars and carbohydrates seem to weaken the adrenals, amino acids seem to strengthen them. Nutritional supplements such as digestive enzymes, betaine HCL, and hydrolyzed collagen are often good supporting nutrients for the GI tract at this stage to help speed up food metabolism, but their effectiveness is often blunted unless the underlying adrenal weakness is repaired.
As the collagen structure of internal organs break down, their functions are compromised. For example, gastrointestinal track motility and contraction forces are reduced. Adrenal Exhaustion is often associated with a poor ability to digest proteins. Common symptoms during this phase of Adrenal Fatigue include constipation, indigestion and irritable bowel syndrome. The amount of acid production may not be sufficient to help break down foods, resulting in further improper digestion and assimilation of nutrients. At the ortho-molecular level, cells are deprived of the much needed nutrients despite a healthy diet with balanced macro-nutritional factors.It is no surprise that secondary fibromyalgia and chronic fatigue syndrome are commonly associated with Adrenal Exhaustion. Many have postulated that Adrenal Fatigue often precedes fibromyalgia and chronic fatigue. There is no doubt, clinically, that Adrenal Exhaustion contributes to the overall fibromyalgia chronic fatigue picture, no matter what the cause. Proteins are made up of amino acids. Just as sugars and carbohydrates seem to weaken the adrenals, amino acids seem to strengthen them. Nutritional supplements such as digestive enzymes, betaine HCL, and hydrolyzed collagen are often good supporting nutrients for the GI tract at this stage to help speed up food metabolism, but their effectiveness is often blunted unless the underlying adrenal weakness is repaired. Cortisol, DHEA, testosterone and estrogen are all produced in the adrenals. Decreased levels of each of these hormones and reduced adrenal function have been linked to depression. It comes as no surprise that Adrenal Exhaustion is strongly associated with increased fears, anxiety, depression, brain fog, and difficulties in concentrating. People will often have less tolerance than they normally do and are easily frustrated.Brain fog, another symptom of Adrenal Fatigue, is a mental state where memory is clouded and unclear. It is not a state of loss of memory, immediate or past. It is a state where memory appears to be “so close and yet so far” in terms of the recollection ability. Examples include the inability to recall where keys are placed, what was done yesterday, difficulty in concentrating, difficulty in memorizing things such as telephone numbers, and confusion. Long-term memory, however, remains intact.
Cortisol, DHEA, testosterone and estrogen are all produced in the adrenals. Decreased levels of each of these hormones and reduced adrenal function have been linked to depression. It comes as no surprise that Adrenal Exhaustion is strongly associated with increased fears, anxiety, depression, brain fog, and difficulties in concentrating. People will often have less tolerance than they normally do and are easily frustrated.Brain fog, another symptom of Adrenal Fatigue, is a mental state where memory is clouded and unclear. It is not a state of loss of memory, immediate or past. It is a state where memory appears to be “so close and yet so far” in terms of the recollection ability. Examples include the inability to recall where keys are placed, what was done yesterday, difficulty in concentrating, difficulty in memorizing things such as telephone numbers, and confusion. Long-term memory, however, remains intact.
Brain fog usually is transient in its duration, lasting anywhere from hours to days, and in advanced cases, can become chronic. The exact pathophysiology is unclear. Most people complaining of brain fog usually have concurrent Adrenal Fatigue or some form of hormonal imbalance. When the body is decompensated, the ability to metabolize nutrients, foods, and medications will be reduced. Some of the metabolites are fat-soluble. However, the brain is lipophilic and has a tendency to attract these metabolites, usually released from the liver. The metabolites circulate to the brain and have the tendency to stay there instead of circulating out of the body quickly. This is a postulated thesis that excessive metabolite build up in the brain over time impedes brain function, resulting in a state called brain fog.
Brain fog usually disappears as the body’s detoxification system improves. This usually happens spontaneously as adrenal function strengthens. However, if the adrenal system is not performing optimally, brain fog may stay for a long time. Some people try to do various types of detoxification, thinking that this will help combat their Adrenal Fatigue. Sometimes it does, but most of the time, a poorly thought out detoxification program can lead to worse brain fog due to retoxification reaction. During the detoxification process, more metabolites that are toxic can be released into the bloodstream, accompanied by symptoms such as fever, muscle and joint pain, and general malaise. Those who are already weak and in the more advanced stages of Adrenal Fatigue may find themselves in an adrenal crisis that is triggered by toxic metabolites, which, have not been cleared out of the body in a timely manner. Getting worse or failing to improve after undergoing a detoxification program is therefore often a sign of underlying adrenal weakness.
There is no medicine to relieve brain fog and most nutritional supplements that enhance liver function and encourage cleansing in the body tend to make the condition worse off. The body is too exhausted to process the toxins that were released during a detoxification process at this stage of Adrenal Exhaustion.
 Hormonal System Imbalance. Key hormones associated with Adrenal Exhaustion include epinephrine (adrenalin), norepinephrine, estrogen, testosterone, melatonin, progesterone, and thyroid.
Hormonal System Imbalance. Key hormones associated with Adrenal Exhaustion include epinephrine (adrenalin), norepinephrine, estrogen, testosterone, melatonin, progesterone, and thyroid.

It comes as no surprise that most post-menopausal women who are experiencing hair loss have an adrenal function problem. Velvety, light-brown-to-black markings usually on the neck, under the arms or in the groin, are associated with high insulin levels (acanthosis nigricans).
In males, low libido is invariably an important sign of Adrenal Exhaustion. The body is in the process of preparing itself for survival due to the onset of Adrenal Fatigue. Production of hormones is deemed less important by the body and reproductive hormones are shunted to produce cortisol to ensure survival. Sex drive is reduced in both men and women, while menstrual cycle irregularity becomes common. Miscarriage prevalence is also increased. Long term androgen excess also increases the risk of infertility, cardiovascular disease, hypertension, osteoporosis, uterine cancer, and pituitary adenoma.
 Many suffering from Adrenal Exhaustion will report having low blood pressure as well as a salt craving. The low blood pressure is due to the reduced amount of fluid in the body and the salt craving is because the body is in an absolute deficiency of sodium. Both are due to the lack of aldosterone. In order to compensate for this, potassium is leaked out of the cells so that the sodium to potassium ratio remains constant. The loss of potassium will be less than that of sodium, and as a result, the potassium to sodium ratio is increased. This imbalance causes another set of metabolic problems further complicating the picture and the effects of Adrenal Fatigue.
Many suffering from Adrenal Exhaustion will report having low blood pressure as well as a salt craving. The low blood pressure is due to the reduced amount of fluid in the body and the salt craving is because the body is in an absolute deficiency of sodium. Both are due to the lack of aldosterone. In order to compensate for this, potassium is leaked out of the cells so that the sodium to potassium ratio remains constant. The loss of potassium will be less than that of sodium, and as a result, the potassium to sodium ratio is increased. This imbalance causes another set of metabolic problems further complicating the picture and the effects of Adrenal Fatigue.
Those suffering from Adrenal Exhaustion, therefore often have a low body fluid volume accompanied by a salt craving due to absolute deficiency in sodium as well as having a normal to high level of potassium. While lost fluids in the body should be replaced, this has to be done carefully and slowly, over a period of days if necessary. When the lost fluid is replaced too quickly without adequate sodium, the amount of sodium in the body may be diluted, resulting in an even lower sodium concentration. Sometimes the replacement is gradual but the body over-reacts, leading to sub-clinical dilutional hyponatremia. Laboratory measurement of the common electrolytes may be normal but the patient will present full-blown signs of hyponatremia, including confusion, lethargy, nausea, headache, seizure, weakness, and restlessness. Those who are in this state may find themselves visiting the Emergency Room for these disturbing symptoms only to be told that all is normal after an extensive work up.
 The body is now in turmoil, confused, and is thrown into disarray. Secondary functions such as the regulation of electrolytes take a back seat and their modulation is compromised. Without a fine modulation of the electrolyte mechanism in place, the body goes through wild swings and is easily dehydrated. Unless the overall fluid load is maintained, sub-clinical dehydration occurs and symptoms of Adrenal Exhaustion will get worse. This is why hydration is so important in fighting Adrenal Fatigue. Many will carry water bottles with them wherever they go to ensure that their hydration is not compromised. However, in some people, the body will sometimes over-react and trigger a state of sub-clinical dilutional hyponatremia (with confusion, headache, etc) even though they have normal laboratory electrolyte levels. This is when the amount of sodium falls relative to the increase in the amount of fluid and is a no-win situation for the sufferer. Maintaining the proper balance of solute and fluid requires extensive clinical experience when dealing with Adrenal Fatigue, which might well be beyond most specialists’ abilities, especially when the laboratory tests look normal while symptoms persist.
The body is now in turmoil, confused, and is thrown into disarray. Secondary functions such as the regulation of electrolytes take a back seat and their modulation is compromised. Without a fine modulation of the electrolyte mechanism in place, the body goes through wild swings and is easily dehydrated. Unless the overall fluid load is maintained, sub-clinical dehydration occurs and symptoms of Adrenal Exhaustion will get worse. This is why hydration is so important in fighting Adrenal Fatigue. Many will carry water bottles with them wherever they go to ensure that their hydration is not compromised. However, in some people, the body will sometimes over-react and trigger a state of sub-clinical dilutional hyponatremia (with confusion, headache, etc) even though they have normal laboratory electrolyte levels. This is when the amount of sodium falls relative to the increase in the amount of fluid and is a no-win situation for the sufferer. Maintaining the proper balance of solute and fluid requires extensive clinical experience when dealing with Adrenal Fatigue, which might well be beyond most specialists’ abilities, especially when the laboratory tests look normal while symptoms persist.
The above is just one example as it comes to electrolyte imbalance in Adrenal Exhaustion. It is not hard to imagine how the body is literally overwhelmed just by looking at the hyperactive disequilibrium occurring in almost every organ system. One analogy to illustrate the effect on Adrenal Fatigue is to imagine a large forest fire out of control with a limited number of firefighters on hand. While the firefighters are able to keep the fire from burning down key buildings, there are not enough fire fighting resources to put the entire fire out 100 percent. As such, the fire is controlled 10 percent to 20 percent at best while the rest of the forest continues to burn. Sooner or later, the few fire fighters will become exhausted and collapse, unless help is rendered.
As we enter into this phase, single system breakdown now affects other systems, creating a domino effect of downward spiral decompensatory effects. Let us take a look at how this works:
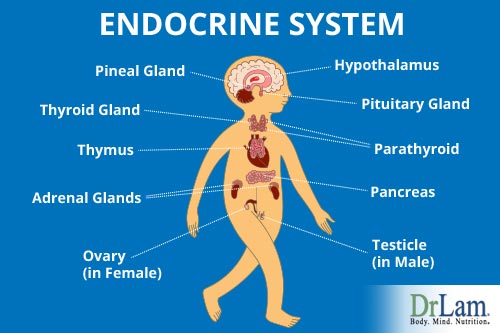
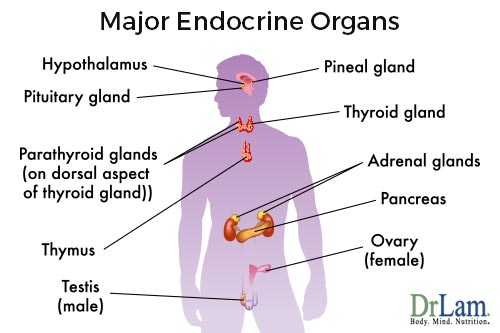 The endocrine system is made up of eight different glands located strategically throughout the body. Three of the most important ones are the ovaries, the adrenals and the thyroid gland in the female and the adrenal and thyroid glands in the male.
The endocrine system is made up of eight different glands located strategically throughout the body. Three of the most important ones are the ovaries, the adrenals and the thyroid gland in the female and the adrenal and thyroid glands in the male.
Controls for the adrenal and ovarian system starts at the hypothalamus. Specifically, the adrenal glands are regulated through the Hypothalamus-Pituitary-Adrenal (HPA) axis. Ovarian hormones are regulated through the Hypothalamus-Pituitary-Ovarian axis. Each of the end organs (adrenals, thyroid, and ovaries) produces a variety of hormones that further exerts its effects on the rest of the body. They all play a role in preventing or combating Adrenal Fatigue. In addition, each of the end organs is tied to other organ systems hormonally via a series of networks or axes.
One such intricate hormonal axis ties in the adrenals, the thyroid and the ovaries and it is called the Ovarian Adrenal Thyroid (OAT) axis in the female and the Adrenal Thyroid (AT) axis in the male. What happens to one organ will affect other organs physiologically, clinically, or sub-clinically. These organs are therefore intimately and hormonally co-dependent on one another for optimal function. If the adrenal glands are weak, there is often concurrent thyroid malfunction (in males) and menstrual cycle irregularity in females. Similarly, an under-active thyroid often makes Adrenal Fatigue worse. Lastly, females who suffer from ovarian hormonal imbalance such as estrogen dominance will often have their pre-existing sub-clinical hypothyroidism exacerbated.
All three end organs must be in a state of optimum balance for a woman or man to feel good. Imbalance of the OAT or AT axis leads to a myriad of conditions that are annoying in their mildest form, and incapacitating when severe. As Adrenal Exhaustion deepens, these axes become more unbalanced.
Common complaints of those suffering from OAT axis imbalance include a mixture of symptoms suggestive of concurrent decompensation of the adrenals, the thyroid, and the ovaries. Presenting symptoms in females are suggestive of Adrenal Fatigue, estrogen dominance, and hypothyroidism concurrently and they include insomnia, chronic fatigue, joint pain, exercise intolerance, brain fog, sugar intolerance, diabetes, dry skin, feelings of being cold, fatigue, slow metabolism, inability to lose weight, PMS, endometriosis, irregular menstrual cycle, fibrocystic breast disease, anxiety, depression, and accumulation of fat at the waistline. Similar symptoms are present in males, with low libido replacing the variety of ovarian system dysfunction manifestations.
The adrenal glands are usually the first in the order of endocrine functions to breakdown in a stressful environment that has overwhelmed the body’s normal compensatory response. It is followed by the insulin-producing portion of the pancreas, then the thyroid, ovaries, parathyroid pineal, pituitary, and finally, the link to the autonomic nervous system, the hypothalamus. Unfortunately, Adrenal Fatigue is frequently overlooked due to the lack of standardized lab testing to detect the condition. As a result, it is only considered seriously, when the patient is already severely decompensated, with concurrent severe ovarian and thyroid involvement. Even when detected, there is inadequate attention paid to the often concurrent ovarian and thyroid imbalance in what is a full blown state of ovarian-adrenal-thyroid axis imbalance.
 When Adrenal Exhaustion triggers a hormonal axis imbalance, patients and physicians alike can easily be overwhelmed. Due to the lack of clinical training on recognizing this axis, single-organ-focus physicians often find themselves treating symptoms of the thyroid or ovarian systems while inadvertently ignoring adrenal dysfunction.Let us take a look at how this can lead to devastating effects.
When Adrenal Exhaustion triggers a hormonal axis imbalance, patients and physicians alike can easily be overwhelmed. Due to the lack of clinical training on recognizing this axis, single-organ-focus physicians often find themselves treating symptoms of the thyroid or ovarian systems while inadvertently ignoring adrenal dysfunction.Let us take a look at how this can lead to devastating effects.
In the early stages of Adrenal Fatigue, cortisol output is high as the body attempts to neutralize the stress by producing more of it. However, when too much cortisol is produced, it will have multiple undesirable effects. For example, cortisol will block progesterone receptors, making them less responsive to progesterone. Progesterone normally produced by the adrenals will come to a halt in favor of cortisol production. Insufficient progesterone production leads to an imbalance between estrogen and progesterone. With reduced progesterone to offset the estrogen, the body may experience estrogen dominance. It is no coincidence that we see a proliferation of conditions associated with excessive estrogen such as PMS, fibroids, and pre-menopausal syndrome when women reach their mid thirties and early forties.
As mentioned earlier, Adrenal Exhaustion generally leads to a state of sub-clinical or clinical hypothyroidism.The thyroid gland acts like the body’s barometer and its main function is to help cells convert oxygen and foods into energy. The thyroid gland regulates the heart rate, blood pressure, body temperature, metabolism, and growth and it is intricately related to the ovarian and adrenal systems. In Adrenal Exhaustion, down-regulation will kick in for survival and thyroid hormones T4 and T3 will be down, while the levels of rT3 and thyroid binding globulin (TBG) will go up. Little attention is paid to rT3 which plays a critical role in balancing T3. RT3 must be displaced by the proper biologically active T3 if thyroid metabolism is to normalize. Patients taking either levothyroxine (L-thyroxin), USP (e.g., Synthroid, Levoxyl), or desiccated thyroid USP (e.g., Armour Thyroid, Westhroid, Naturethroid) may not have sufficient T3 to displace the excess accumulation of rT3 and this leads to a net shortfall of T3. The patient may be bathing in T4 but will still be starving for the biological active T3. Symptoms of hypothyroidism will remain despite an adequate level of T4 in the serum and a normal TSH level. The patient’s basal body temperature almost always is low and will stay low. Increasing dosage of thyroid replacement medication will not help because the body is not getting the T3 that the body really needs. Unsuspecting physicians may try to treat unresolved symptoms by increasing the medication dosage. Not only will this fail to produce the desired clinical results but it makes the overall condition even worse. When the medication dosage is raised, the already weak adrenal glands, along with the rest of the body, are put into over-drive. This extra burden and load can unmask Adrenal Fatigue, worsen Adrenal Exhaustion, and at times trigger an adrenal crisis.
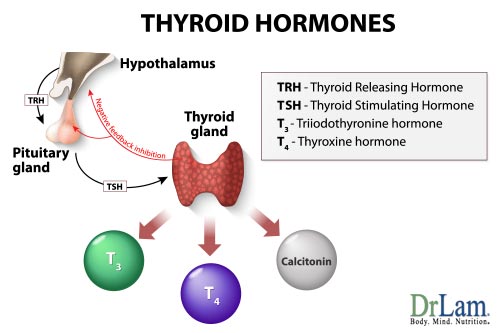 Although some available drugs deliver T3 (Cytomel, for example) or combine T4 with T3 (Thyrolar), the T3 in these preparations are not released slowly. As a result, patients will continue to suffer from the symptoms that result from uneven T3 distribution. Unfortunately, very few physicians are knowledgeable about slow-release T3 and its proper usage to combat this aspect of Adrenal Fatigue.
Although some available drugs deliver T3 (Cytomel, for example) or combine T4 with T3 (Thyrolar), the T3 in these preparations are not released slowly. As a result, patients will continue to suffer from the symptoms that result from uneven T3 distribution. Unfortunately, very few physicians are knowledgeable about slow-release T3 and its proper usage to combat this aspect of Adrenal Fatigue.
Due to its relative ease of detection, thyroid dysfunction is often the first to be treated with subsequent thyroid replacement therapy. Unfortunately, most patients treated this way will remain symptomatic. Not first, considering adrenal fortification is a common mistake and often leads to a worsening state of OAT axis imbalance and thyroid dysfunction. The reason is simple. Thyroid replacements normally tend to increase the body’s metabolic function. However, raising the basal metabolic rate is akin to putting all systems of the body into overdrive. An already weak adrenal system may not be able to tolerate this. Thyroid replacement can therefore further weaken pre-existing adrenal weakness and can also unmask sub-clinical Adrenal Fatigue or act as a trigger to precipitate an adrenal crisis. Those who have thyroid problems but fail to improve with medications should always investigate the adrenals for possible concurrent dysfunction. Low adrenal function therefore can worsen thyroid function.
In summary, Adrenal Exhaustion often leads to low libido and low thyroid function concurrently in males. In females, exhausted adrenals will worsen the ovarian system and thyroid function. Hypothyroidism in turn exacerbates adrenal weakness and blunts the ovarian hormonal responses. The body is thrown into a vicious downward cycle of cascading decompensation. This is often made worse by medications and improper treatment protocols.
In addition to major symptoms of OAT axis imbalance consisting of hypothyroidism, estrogen dominance and Adrenal Fatigue, other organ systems are also frequently involved, especially in this phase of Adrenal Exhaustion. For example, the processing and assimilation of nutrients are often compromised. Absorption of nutrients in the GI track is reduced as leaky gut, irritable bowl, food sensitivity, and internal dysbiosis overwhelm the normal gut flora. Liver function is reduced, despite test results showing normal liver function. Good nutrients, if not processed and metabolized properly, become toxic. Toxic metabolites will circulate inside the body, and if not properly cleared, they can lead to brain fog, joint pain, skin rashes, allergies, muscle discomfort, and multiple chemical sensitivities, among many other symptoms. No organ system is spared of dysfunction when this axis is not well balanced. This sets the stage for multi-organ system failure, leading to weakened adrenals that may collapse totally.
 Because this OAT axis imbalance is seldom recognized by conventionally trained physicians, clinicians often focus their attention to either helping the thyroid or the ovarian system to recover. Hormonal replacement, whether natural or synthetic, is often prescribed. Those with OAT axis imbalance will often find a dull response over time with this single focus approach, which invariably leads to an often unrecognizable change in the other two organs. For example, if thyroid medication is administered, it is not uncommon to see concurrent menstrual irregularities, a function of ovarian hormones, and reduced ability to deal with stress and worsening fatigue, a function of the adrenals. The inexperienced physician is at a loss as to why recovery is blunted as the underlying causes of Adrenal Fatigue have not been addressed. Patients are discouraged and disappointed with their health professionals. Ultimately, the patients prescribed with an increasing dose of medications will give up after they have failed to reach their therapeutic goal.
Because this OAT axis imbalance is seldom recognized by conventionally trained physicians, clinicians often focus their attention to either helping the thyroid or the ovarian system to recover. Hormonal replacement, whether natural or synthetic, is often prescribed. Those with OAT axis imbalance will often find a dull response over time with this single focus approach, which invariably leads to an often unrecognizable change in the other two organs. For example, if thyroid medication is administered, it is not uncommon to see concurrent menstrual irregularities, a function of ovarian hormones, and reduced ability to deal with stress and worsening fatigue, a function of the adrenals. The inexperienced physician is at a loss as to why recovery is blunted as the underlying causes of Adrenal Fatigue have not been addressed. Patients are discouraged and disappointed with their health professionals. Ultimately, the patients prescribed with an increasing dose of medications will give up after they have failed to reach their therapeutic goal.
Because the presenting complaints are often prominent in relation to one of the three organ systems, physicians are frequently misled. For example, PMS may be the dominant symptom, leading clinicians to focus on treating the sexual hormones. If physical tiredness is the predominant complaint, the focus is usually on the thyroid gland. The adrenals are frequently passed over as insignificant. Conventionally trained physicians often resort to the use of anti-depressants, thyroid replacements and ovarian hormones such as estrogen and progestin (or even natural hormones) without careful consideration of OAT (or AT axis) imbalance. However, the prescribed medicines can worsen the imbalance as they mask the underlying problem. Because laboratory test results can be misleading, many health care professionals not alerted to this condition, might end up prescribing medications based on laboratory results rather than looking at the bigger picture – to see what the patient is really going through and what the symptoms are really telling us. Many sufferers will embark on programs of hormonal replacement only to find that such endeavors become ineffective over time. In women, symptoms of estrogen dominance like hot flashes, weight gain at the hips, water retention, and moodiness are common. In men, continued low libido, lack of energy and insomnia will compromise normal daily living. Successful recovery from this phase of Adrenal Fatigue should start with repairing the adrenals with concurrent attention to the thyroid and the ovarian systems. Dramatic results can be seen with the right program but the key here is to repair the adrenals first.
Phase B dysfunction of Adrenal Exhaustion involves disruption of the major adrenal related hormonal axis. The body as a whole, however, is still functioning relatively well. Despite sub-clinical hypothyroidism, low energy, estrogen dominance, irregular periods (in females) and low libido, critical body functions remain relatively intact.
 As the adrenals decompensate and enter into Phase C of Adrenal Exhaustion, the body weakens further, triggering its various reserve systems to spring into action as the body loses its homeostasis and equilibrium.
As the adrenals decompensate and enter into Phase C of Adrenal Exhaustion, the body weakens further, triggering its various reserve systems to spring into action as the body loses its homeostasis and equilibrium.
Let us now examine this more deeply. Homeostasis is derived from Greek, meaning to stand equally and is used to describe a theory of physiology expounded by Claude Bernard. The theory was that, in order for a closed system to maintain equilibrium with its surrounding environment, the system requires many minute exchanges and dynamic adjustments internally to maintain the status quo. Our body is comprised of more than 70 trillion cells. To be in optimum health, a cell and by extension the body must maintain its equilibrium or homeostasis with its surrounding environment. At the cellular level, basic chemical and electrical transactions occur. For homeostasis to occur, the cells must be able to excrete waste and take in new materials in equal measure. Regulatory systems such as the negative feedback loop and the autonomic nervous system are needed to maintain this equilibrium. Cellular equilibrium homeostasis can therefore, be defined as the stability of physiological systems that maintain life. Without this equilibrium, the body will not be able to perform such mundane function as standing up, maintaining stable body temperature and heart rate, for example. As the needs of cells will change depending on the stress placed upon them, such regulatory systems are normally activated automatically and this is an unconscious event. Without our knowledge, these regulatory systems keep our body in perfect harmony internally and prevent Adrenal Fatigue. These systems are jeopardized in Phase C of Adrenal Exhaustion.
The key regulatory systems for internal equilibrium are the nervous system and the endocrine system. While the functions of both of these systems may be compromised in earlier phases, they enter into a steep slope of declining function during this phase of Adrenal Fatigue, with dire consequences, as we shall see. In layman’s terms, the internal thermostat of the body is broken. In order to maintain normal function, the compensatory systems of the body comprising the neurological and endocrine systems are activated. Unfortunately, these reserve and compensatory systems are crude at best and they lack the fine-tune capabilities of the regular systems. The key functions of the body are saved but there is a price to be paid as a variety of side effects surface. In a way, these side effects are the body’s way of alerting us that it is in trouble. Often, instead of taking advantage of these hints to help us gauge the level of dysfunction and use them as markers during the recovery process, the tendency is to turn to the quick fix approach of suppressing these symptoms. Over time, this only weakens the adrenals as well as the other systems involved.
In addition to Phase A symptoms of Adrenal Fatigue such as salt craving, insomnia, and low blood pressure at rest, and Phase B symptoms of Adrenal Fatigue such as feeling cold, sluggish, irregular periods, PMS, low libido, acne and hypoglycemia, the typical Phase C Adrenal Exhaustion patient will also complain of one or more of the following: sudden onset of anxiety attacks, impending doom at rest, sudden onset of heart palpitations despite a normal cardiac function, sudden onset of dizziness and lightheadedness at rest, waking up in the middle of the night for no reasons and the inability to go back to sleep, sudden onset of fragile emotional states such as crying for no apparent reason, fragile reactive fluid state with edema and sodium imbalance, a sudden onset of fluctuating blood pressure, orthostatic hypotension, POTS, cardiac arrhythmia and orthostatic intolerance.
Dysfunction of the Autonomic Nervous System (ANS) is responsible for many of the above Phase C Adrenal Fatigue symptoms. Let us examine this more closely.
 The nervous system of the body is divided into the central (brain and spinal cord) and the Peripheral Nervous System. The Peripheral Nervous System of the body is in turn divided into two parts: the Somatic Nervous System that regulates skeletal muscle functions that help us deal with the outside world and the Autonomic Nervous System (ANS) that regulates functions of the smooth muscles and glands within the body for proper inner world workings. The ANS is further divided into the Parasympathetic Nervous System (PNS), the Sympathetic Nervous System (SNS) and the Adrenomedullary Hormonal System (AHS). The PNS regulates the vegetative processes such as urination and digestive function. Dysfunction of the PNS leads to a wide variety of illnesses including abnormal gastric acid secretion, reduced gut motion, erectile dysfunction, and loss of urinary control and bowel movement irregularities. The SNS regulates the unconscious housekeeping functions of the body, including blood pressure, body temperature, force of the heart-beat, and heart rate. The AHS (also called the sympathetic adrenergic system) regulates the emergency and distress functions such as those responsible for the body’s “fight or flight” response and it has properties similar to SNS, plus more. It is also activated in fainting, shock, extreme fear, hypoglycemia, and low body temperature. The other parts of the ANS include the Enteric Nervous System (ENS), which regulates enteric functions and the Sympathetic Cholinergic System (SCS) that regulates sweating.
The nervous system of the body is divided into the central (brain and spinal cord) and the Peripheral Nervous System. The Peripheral Nervous System of the body is in turn divided into two parts: the Somatic Nervous System that regulates skeletal muscle functions that help us deal with the outside world and the Autonomic Nervous System (ANS) that regulates functions of the smooth muscles and glands within the body for proper inner world workings. The ANS is further divided into the Parasympathetic Nervous System (PNS), the Sympathetic Nervous System (SNS) and the Adrenomedullary Hormonal System (AHS). The PNS regulates the vegetative processes such as urination and digestive function. Dysfunction of the PNS leads to a wide variety of illnesses including abnormal gastric acid secretion, reduced gut motion, erectile dysfunction, and loss of urinary control and bowel movement irregularities. The SNS regulates the unconscious housekeeping functions of the body, including blood pressure, body temperature, force of the heart-beat, and heart rate. The AHS (also called the sympathetic adrenergic system) regulates the emergency and distress functions such as those responsible for the body’s “fight or flight” response and it has properties similar to SNS, plus more. It is also activated in fainting, shock, extreme fear, hypoglycemia, and low body temperature. The other parts of the ANS include the Enteric Nervous System (ENS), which regulates enteric functions and the Sympathetic Cholinergic System (SCS) that regulates sweating.
The combination of AHS and SNS constitutes the sympathoadrenal system (SAS). Maintaining a normal balance of the SAS within the ANS is vital to optimal body function and homeostasis. This is of particular importance in the case of Adrenal Exhaustion because it is the dysregulation of the messengers of these two systems, namely adrenaline (also called epinephrine) in the case of AHS and norepinephrine (also called noradrenaline) in the case of SNS, that is the hallmark of Phase C Adrenal Exhaustion symptoms.
 The sympathoadrenal system is one of the major pathways mediating physiological responses in the body and plays an important role in the regulation of heart rate, blood pressure, glucose, sodium and other key physiological and metabolic processes such as the fight or flight response. The SAS is affected by many disease states and is able to preserve homeostasis by corrective physiological responses. Many therapeutic agents are either adrenergic activators or inhibitors.
The sympathoadrenal system is one of the major pathways mediating physiological responses in the body and plays an important role in the regulation of heart rate, blood pressure, glucose, sodium and other key physiological and metabolic processes such as the fight or flight response. The SAS is affected by many disease states and is able to preserve homeostasis by corrective physiological responses. Many therapeutic agents are either adrenergic activators or inhibitors.
The two components of the SAS are the SNS and the AHS. Norepinephrine is a neurotransmitter secreted under the control of the SNS. Adrenaline is a hormone secreted from the adrenal medulla, which is under the control of the Adrenomedullary Hormone System (AHS) and deals with emergency functions of the body. Norepinephrine is the key neurotransmitter responsible for regulating blood pressure and heart rate at rest. Adrenaline is also present, though in a much reduced amount.
Chemically, adrenaline is the chemical son of norepinephrine, and in turn, norepinephrine is the chemical son of dopamine. These three chemicals fall within a family called catecholamines and they represent three different ways the body is regulated internally. Adrenaline is a hormone that has wide ranging effect throughout the body as it is transported by the blood stream once it is released from the adrenal glands. Norepinephrine is a neurotransmitter released from the nerves of the SNS and acts mainly locally on nearby target cells such as the heart. For example, norepinephrine released by the SNS into the heart regulates heart rate and its presence in the blood stream has to be in high concentration before it can exert its effects as a hormone. Finally, dopamine appears to have dual properties. Peripherally, in the gut, adrenal and kidneys where it is produced in and released from, dopamine acts on the same type of cells in the immediate vicinity. In the central nervous system, dopamine behaves like a neurotransmitter.
Low levels of norepinephrine are associated with loss of alertness, poor memory and depression. Norepinephrine appears to be the neurotransmitter of “arousal” and it is for this reason that medications for depression and ADHD often target both dopamine and norepinephrine in an attempt to restore them to normal levels. Mild elevations in our norepinephrine level produce heightened arousal, something known to be produced by stimulants. This arousal is considered pleasurable and several “street drugs” such as cocaine and amphetamines work by increasing the brain level of norepinephrine. Moderately high levels of norepinephrine create a sense of arousal that makes us uncomfortable, such as anxiety, increased startle reflex, jumpiness, fear of crowds and tight places, impaired concentration, restless sleep, and physical changes. The physical symptoms may include rapid fatigue, muscle tension/cramps, irritability and a sense of being on edge. Almost all anxiety disorders involve elevation in norepinephrine levels. Severe and sudden increases in norepinephrine levels are also associated with panic attacks.
Adrenaline (epinephrine) is one of the most powerful vasopressor (causing a rise in blood pressure) drugs known. It increases the strength of heart muscle contractions as well as the heart rate. It constricts blood vessels and veins, and is also a powerful bronchodilator and inhibits the release of histamines, which are triggered by allergic reaction. Finally, adrenaline is responsible for the body’s “fight or flight” response.
At rest, plasma concentrations of adrenaline and norepinephrine are low (less than 1 microgram per liter), but they can rise under certain physiological (adaptation) or pathological conditions. For example, when one goes from the supine to the standing position, norepinephrine concentration increases two fold. In patients with pheochromocytoma plasma, catecholamines can rise transiently and reach high levels.
The actions of adrenaline and norepinephrine are generally similar, although they differ from the other in certain of their effects. Norepinephrine constricts most blood vessels, while adrenaline causes constriction in many networks of minute blood vessels but dilates the blood vessels in the skeletal muscles and liver.  Both hormones increase the rate and force of contraction of the heart, thus increasing the output of blood from the heart and increasing the blood pressure under normal conditions. These two hormones also have important metabolic actions. Adrenaline stimulates the breakdown of glycogen into glucose in the liver resulting in the rise of blood sugar level. Both hormones increase the level of circulating free fatty acids. The extra amounts of glucose and fatty acids can then be used by the body as fuel in times of stress or danger, when increased alertness or exertion is required.
Both hormones increase the rate and force of contraction of the heart, thus increasing the output of blood from the heart and increasing the blood pressure under normal conditions. These two hormones also have important metabolic actions. Adrenaline stimulates the breakdown of glycogen into glucose in the liver resulting in the rise of blood sugar level. Both hormones increase the level of circulating free fatty acids. The extra amounts of glucose and fatty acids can then be used by the body as fuel in times of stress or danger, when increased alertness or exertion is required.
Because adrenaline is much more powerful than norepinephrine, its deployment is more tightly controlled and it is released in great amount during times of extreme distress. It is sometimes called the emergency hormone because it is released during stress and its stimulatory effects will fortify and prepare an animal for either flight or fight response. Chronic or acute stress leading to Adrenal Exhaustion increases AHS activation. A rise in the absolute level of adrenaline in the body will cause the following: increase in heart rate, increase in blood sugar, increase in respiration, reduction in serum potassium, relaxation of skeletal muscle blood vessels, increase in energy, increase in emotional sweating, constriction of skin blood vessels (pallor), relaxation of the gut and trembling. This adrenaline overload, along with norepinephrine, will worsen the existing ANS imbalance that is already happening in earlier phases of Adrenal Exhaustion and will trigger an additional host of dysfunctions, above and beyond those already experienced in the earlier stages of Adrenal Fatigue.
In healthy people, excess adrenaline released from the adrenal glands during stress is quickly swept up by efficient adrenaline transporters that carry away these undesirable hormones before it can wreak havoc inside the body. For example, standing requires blood vessels to contract to keep gravity from allowing all your blood from pooling in your legs. This is accomplished through the release of small amounts of adrenaline. The body releases just the right amount of this hormone throughout the day as we move around and change positions. However, excessive amounts of adrenaline are cleared out of the body. The body’s blood pressure is thus maintained in a normal state. In Phase C of Adrenal Exhaustion, activation of the SAS will lead to the release of a larger amount of adrenaline and norepinephrine, which will remain in circulation for longer than usual duration before they are inactivated.
 Blood pressure in the Adrenal Exhausted state is usually below normal level but it can abruptly increase and stay high if a large amount of adrenaline is released quickly into the bloodstream. At the same time, the heart rate may be elevated as well. Consistent high levels of norepinephrine and epinephrine will also lower the threshold of normal cardiac rhythm, triggering abnormal cardiac arrhythmias such as atrial fibrillation. Adrenaline released during an emergency response, is usually self-limiting in fit people. However, in Phase C of Adrenal Exhaustion, this release can become exaggerated in certain people. The physiological mechanisms of the pathway is not fully known but research studies are pointing to the loss of the more stable negative feedback loop of regulatory function in favor of the less stable and ultimately destructive positive feedback loop response as a possible etiology.
Blood pressure in the Adrenal Exhausted state is usually below normal level but it can abruptly increase and stay high if a large amount of adrenaline is released quickly into the bloodstream. At the same time, the heart rate may be elevated as well. Consistent high levels of norepinephrine and epinephrine will also lower the threshold of normal cardiac rhythm, triggering abnormal cardiac arrhythmias such as atrial fibrillation. Adrenaline released during an emergency response, is usually self-limiting in fit people. However, in Phase C of Adrenal Exhaustion, this release can become exaggerated in certain people. The physiological mechanisms of the pathway is not fully known but research studies are pointing to the loss of the more stable negative feedback loop of regulatory function in favor of the less stable and ultimately destructive positive feedback loop response as a possible etiology.
As mentioned earlier, adrenaline is a hormone that is stimulatory in nature. Symptoms of excessive adrenaline include heart palpitation, irritability and anxiety. Less common symptoms are dizziness, cold sweats, brain fog and orthostatic hypotension.
In addition to possible adrenaline overload, those with weak adrenals may have a reduced capacity to clear excessive unwanted adrenaline and its metabolites from the body, leading to the toxic build-up of metabolites and manifestation of symptoms such as fatigue, jitteriness, and nervousness, brain fog, anxiety, insomnia and fatigue.This low-clearance state is especially prevalent in people with weak adrenal glands and the accompanying Adrenal Fatigue. We shall discuss these phenomena in more detail in Phase D.
Defective epinephrine and norepinephrine transporter systems can also worsen the condition and contribute to higher levels of excessive adrenaline because norepinephrine is the chemical father of epinephrine and its level is tied to epinephrine.
Over stimulation of the SAS with resulting adrenaline and norepinephrine overload in the context of Adrenal Fatigue are usually a compensatory reaction of the ANS that is triggered by stress and causes the SAS to be activated and put into overdrive. The resulting cascade of automated responses is called Reactive Sympathoadrenal Response (RSR). Because activation of SAS is a secondary function of Adrenal Exhaustion, it is called reactive. The systems activated are the sympathetic nervous system and the adrenomedullary hormonal system, thus the name sympathoadrenal. The responses generated are usually due to over-stimulation and sometimes because of imbalance as well. The term Reactive Sympathoadrenal Overtone (RSO) is used when the response is due to over-stimulation. In short, the body is bathed in a sea of adrenaline and norepinephrine.
RSR comprises of a myriad of symptoms such as clinical or sub-clinical orthostatic intolerance, fragile blood pressure, inability to stand for a long time, lightheadedness, “spaciness,” tachycardia, CVD, irregular heart rate, temperature intolerance, body fluid and electrolyte imbalance, sweating, fainting, POTS, loss of bowel and urination control, sense of impending doom, and dizziness. Some of these symptoms are due to excessive amounts of adrenaline and norepinephrine while others are due to imbalances between adrenaline and norepinephrine (also called sympathoadrenal imbalance). Some are of unknown etiology. Fainting is a classic example of sympathoadrenal imbalance, while tacycardia is a classic example of sympathoadrenal overtone.
Sympathoadrenal overtone contributes to the development of Cerebral Vascular Diseases (CVD) such as stroke through the effects of catecholamines on the heart, blood vessels, and platelets. Sympathoadrenal activation also modifies the function of circulating platelets through catecholamine-induced changes in hemodynamic factors (increased shear stress), circulating lipids, and inhibition of vascular eicosanoid synthesis.
 In Phase C of Adrenal Exhaustion, the body can become extraordinarily sensitive to stressors. Mundane activities may act as triggers in this phase while they normally do not behave as triggers in early stages of Adrenal Fatigue. It appears that the threshold for stressors to act as triggers is lowered for reasons not well understood. For example,activities such as eating a big meal high in refined carbohydrates, watching an action movie, being exposed to fluorescent lighting, taking a cold drink, prolonged sitting in front of a computer monitor, taking a long car drive, being startled by the phone ringing in a quiet room, performing a short but intense dance or exercise, being exposed to cold or hot temperature that the body is not used to (even though the temperature is within normal comfort zone for the general population), taking an uphill or long walk, being exposed to indirect sunlight, drinking soda pop, tea, or coffee, eating chocolate, and eating food that is hard to digest such as corn, etc. may act as triggers.
In Phase C of Adrenal Exhaustion, the body can become extraordinarily sensitive to stressors. Mundane activities may act as triggers in this phase while they normally do not behave as triggers in early stages of Adrenal Fatigue. It appears that the threshold for stressors to act as triggers is lowered for reasons not well understood. For example,activities such as eating a big meal high in refined carbohydrates, watching an action movie, being exposed to fluorescent lighting, taking a cold drink, prolonged sitting in front of a computer monitor, taking a long car drive, being startled by the phone ringing in a quiet room, performing a short but intense dance or exercise, being exposed to cold or hot temperature that the body is not used to (even though the temperature is within normal comfort zone for the general population), taking an uphill or long walk, being exposed to indirect sunlight, drinking soda pop, tea, or coffee, eating chocolate, and eating food that is hard to digest such as corn, etc. may act as triggers.
While the activation of the SAS ensures the body’s survival by bringing more blood supply to the brain, the fine control of the rest of the body is compromised, including the metabolic, endocrine and central nervous systems.The body, as a result, will experience exaggerated and wild metabolic and hormonal roller-coaster rides with fluctuations in blood sugar level, body temperature, blood pressure, heart rate, sleep, and emotional states. The state of acute adrenal weakness is also known as an adrenal crash. Symptoms of Adrenal Fatigue will become drastically exaggerated during an adrenal crash. Once the SAS is activated, it may take hours or even weeks before the body is able to return to baseline.
Standard medical workups remain unremarkable, as the symptoms tend to remain sub-clinical. The weaker the adrenal function, the longer the recovery time is.
There may be a genetic involvement in this convoluted picture. More research is needed but it is clinically clear that those with weak adrenals have higher tendencies to be more sensitive to excessive adrenaline / norepinephrine and more prone to suffer symptoms resembling sub-clinical dysfunction of the ANS (also called dysautonomia). The weaker the adrenals, the stronger this association will be. Interestingly, dysautonomia is also much more prevalent in those people who suffer from mitral valve prolapse, a very common and benign condition of the heart.Those who suffer from Adrenal Fatigue and mitral valve prolapse should therefore be on special alert for dysautonomia.
 Unless an experienced clinician is on alert, this reactive state can easily be missed and the symptoms will often be dismissed as insignificant. Patients are often started on the failed approach of drugs such as anti-depressants to control the symptoms rather than healing the adrenals and thereby mitigating the effects of Adrenal Fatigue. This is a common mistake. Each symptom is there for a reason; it is the body’s way of alerting us of trouble within. Close attention should therefore be paid to every symptom, as each is a piece in an extensive jigsaw puzzle. Treating the symptom will often mask the underlying pathology and thus miss the big picture.
Unless an experienced clinician is on alert, this reactive state can easily be missed and the symptoms will often be dismissed as insignificant. Patients are often started on the failed approach of drugs such as anti-depressants to control the symptoms rather than healing the adrenals and thereby mitigating the effects of Adrenal Fatigue. This is a common mistake. Each symptom is there for a reason; it is the body’s way of alerting us of trouble within. Close attention should therefore be paid to every symptom, as each is a piece in an extensive jigsaw puzzle. Treating the symptom will often mask the underlying pathology and thus miss the big picture.
Those who are in Phase C of Adrenal Fatigue are often concurrently burdened by worsening symptoms of Phases A and B (severe single organ system dysfunction and hormonal axis imbalance). There is tremendous overlapping of symptomatology among the three phases because they are closely related. Disruption of the ANS (characteristic of Phase C pathology) affects the Hypothalamic-Pituitary-Adrenocortical axis (HPA) that controls adrenal cortex function. As adrenal cortex hormone depletion progresses (Phase A pathology), overall adrenal function is compromised as the cortisol, estrogen, and thyroid functions have become dysregulated, leading to OAT axis imbalance (Phase B pathology).
The HPA axis and the SNS are also interrelated. Stimulating one system tends to inhibit the activity in the other. As the SNS outflow is increased, glucocorticoid released from the adrenal cortex is reduced. In other words, the reactive sympathoadrenal response (RSR) seen in Phase C Adrenal Fatigue with increased secretion of epinephrine and norepinephrine will blunt cortisol and aldosterone output. As a result, salt craving will increase and low blood pressure will become more pronounced, exacerbating Phase A and B Adrenal Fatigue symptoms. Administration of glucocorticoids (such as hydrocortisone) decreases SNS outflow, whereas studies have shown that surgical removal of adrenal glands increases SNS outflow. Paradoxically, glucocorticoids also promote adrenaline output from the adrenal medulla by promoting the activity of the enzyme responsible for converting norepinephrine to epinephrine. Studies have shown that pathological states involving the failure of adrenal cortex often are associated with decreased adrenaline production. The exact mechanism is not known but it is clear that our understanding of how the various hormones affect one another within the adrenal and nervous systems remains in its infancy and that the three phases of Adrenal Exhaustion are intimately related to one another in terms of how one affects the other.
As Phase C Adrenal Fatigue progresses, cortisol and aldosterone levels, already low, will generally go lower. Salt cravings and low blood pressure will become more pronounced and usually get worse. Without sufficient cortisol to blunt the compensatory adrenaline response, the body then becomes susceptible to the ever larger gyrating level of adrenaline and norepinephrine output that can be abrupt as the SAS is activated in the body.As more adrenaline is being released without the dampening effect of cortisol, blood pressure can suddenly rise and spike on a reactive basis, leading to an abrupt onset of intermittent higher than normal blood pressure, anxiety, and heart palpitations. When the rush is over, the body drops back down to a lower than normal level of function, resulting in lower than normal blood pressure, and the patient becomes exhausted. Blood sugar can similarly be affected, with resulting sub-clinical hyperglycemia first leading to a hypoglycemic state characteristic of an unstable blood glucose curve, while blood sugar remains within normal limits by conventional medical standards. It comes as no surprise that the body is constantly drained of energy just having to deal with this never-ending parade of disequilibrium. Because sleep is invariably disrupted, a state of persistent tiredness or chronic fatigue is common as the body is essentially in a “slow down” mode in order to conserve energy.
 In some people, the reactive sympathoadrenal response (RSR) can be exaggerated with levels of epinephrine and norepinephrine output becoming higher and well beyond normal activation. As a result, many feel “wired and tired” at the same time throughout the day. The body is tired and wishes to rest but is at the same time on full alert 24/7. When it is time to sleep, the body is unable to relax and severe sleep insomnia is the norm. Many are nocturnal, unable to sleep at night and only able to catch cat-naps during the day, as the body is in this constant state of high alert. Others may be able to fall asleep after a long time, when the “tired” factor outweighs the “wired” factor. However, this is usually short lived and the tendency is to be awakened after a short rest as the “wired” factor resurges into dominance.
In some people, the reactive sympathoadrenal response (RSR) can be exaggerated with levels of epinephrine and norepinephrine output becoming higher and well beyond normal activation. As a result, many feel “wired and tired” at the same time throughout the day. The body is tired and wishes to rest but is at the same time on full alert 24/7. When it is time to sleep, the body is unable to relax and severe sleep insomnia is the norm. Many are nocturnal, unable to sleep at night and only able to catch cat-naps during the day, as the body is in this constant state of high alert. Others may be able to fall asleep after a long time, when the “tired” factor outweighs the “wired” factor. However, this is usually short lived and the tendency is to be awakened after a short rest as the “wired” factor resurges into dominance.
As the condition deteriorates and the sufferer moves closer to Phase D of Adrenal Fatigue, extreme fatigue sets in as the patient becomes bedridden for a large part of the day. Sleep patterns are often disrupted with sudden onsets of cold sweat from adrenaline rushes along with unstable blood glucose and blood pressure levels. This leads to shortness of breath, anxiety attacks, edema, headache and heart palpations accompanied by a slowing GI system with constipation and inability to assimilate food etc. There will be frequent visits to the Emergency Room (only to be told that all is well and then sent home with anti-depressants). During the day, frequent small meals and severe carbohydrate restriction may be needed to avoid frequent reactive hypoglycemia episodes and their many unpleasant side effects. If not reversed soon, even normal nutritional supplements that have helped earlier will start to fail and in fact, make the condition worse off. The failure may even extend to steroidal medications as severe paradoxical reactions may surface. Those who are in Phase C of Adrenal Fatigue truly live in a state of the “living dead,” abandoned by their physicians and left to self navigate through deep unchartered waters.
 All hormones in the body are interrelated to one another in some form. Many important hormones are dependent on other hormones to work. For example, estrogen is needed for progesterone to work. A minimum level of each hormone is required to be present in the body before basic body functions can begin. As the levels of cortisol and aldosterone hormones fall below the minimum required for normal body function and their output fails, the body may either slow down its normal function or down-regulate the amount needed in order to preserve what is on hand for only the most essential of body functions. The body’s strategy of returning to a simple state of physiologic function is in full force. This down-regulation further reduces vital hormonal output, exaggerating a downward vicious cascade. In this phase, rapid weight loss, gastric disturbance, and severe loss of muscle tone are common; as the body enters into “shut down” mode to further conserve energy. You are in the last stage of Adrenal Fatigue.
All hormones in the body are interrelated to one another in some form. Many important hormones are dependent on other hormones to work. For example, estrogen is needed for progesterone to work. A minimum level of each hormone is required to be present in the body before basic body functions can begin. As the levels of cortisol and aldosterone hormones fall below the minimum required for normal body function and their output fails, the body may either slow down its normal function or down-regulate the amount needed in order to preserve what is on hand for only the most essential of body functions. The body’s strategy of returning to a simple state of physiologic function is in full force. This down-regulation further reduces vital hormonal output, exaggerating a downward vicious cascade. In this phase, rapid weight loss, gastric disturbance, and severe loss of muscle tone are common; as the body enters into “shut down” mode to further conserve energy. You are in the last stage of Adrenal Fatigue.
When the levels of these critical hormones fall below the minimum levels required for basic body function, the organs become severely compromised. Pump failure starts to occur and attempts to prime the pump to regain the footing become very difficult. The threshold level of each hormone varies from person to person. No laboratory test is currently available to help determine this with accuracy. The key to help prevent or reverse this state lies in understanding the patient’s history and observing the clinical presentations with careful attention to minute detail. The patient is often incapacitated and bedridden, requiring assistance to conduct daily activities such as driving, shopping and preparation of meals. The low energy state renders the patient bed-ridden most of the time.
No organ is spared as the body down-regulates throughout all phases of Stage 3. The symptoms may not be new as the phases progresses, but they reach their peak intensity at Phase D.
Let us look at what the high intensity of the symptoms of this phase of Adrenal Fatigue are telling us about our body internally. The first symptoms to show up usually represent the organ system to be turned off first as it is not required for basic survival. Reproduction is considered a luxury and not a vital function when survival is at stake. Libido as a result is lowered. Sex drive becomes non-existence. The thyroid also goes into a slow down mode as the body attempts to reduce the basal metabolic rate (idle speed) to conserve energy. This naturally leads to sluggishness, constipation, and worsening fatigue. Clinical hypothyroidism is common. The gastrointestinal tract as a whole tends to slow down in its assimilation of food. Complex and processed foods become hard to digest and less is absorbed. Digestive enzymes and acid release are reduced. Gastric motility slows. As a result, foods do not churn as much compared to that of a normal healthy person. Poor digestion is common, accompanied by reduced absorption; increased gas, bloating, and constipation. As this happens, the liver and kidney functions are also affected. Both are the clearing houses of the body’s toxins. As liver function slows (though laboratory tests are usually normal), complete breakdown of metabolites becomes compromised. Overall, body clearance of such by-products tends to slow concurrently as toxic metabolite build up occurs as a result. Fat-based metabolites tend to find their way into areas of the body high in fat as they attract each other. Lipophilic organs (organs that like fat) such as the brain have a tendency to attract such fat based metabolites easily. Instead of a normal complete clearance out of the body on a timely basis, such metabolites tend to accumulate instead. Metabolites that accumulate in the brain can lead to and contribute to memory loss, confusion, anxiety, and brain fog. Normal brain function may be impaired if severe. Some accumulate in joints and muscles, leading to muscle pain of unknown origin and joint inflammation. This is just part of the picture.
 The down-regulation or return to simplicity will continue as long as the body sees it as a positive step to conserve energy for survival. As the body further slows down, muscle breaks down to generate energy, leading to an overall net loss of protein and muscle mass. When this happens, the body enters a catabolic state, with overall weight loss and muscle wasting. Fibromyalgia and Chronic Fatigue Syndrome may be triggered. Appetite reduces as the gastrointestinal tract motility slows and gastric capacity reduces. Those with sugar imbalances and insulin resistances are particularly vulnerable to a worsening state. Electrolyte imbalance, especially as it relates to sodium and potassium, becomes common. The myriad of physical symptoms mentioned above is convoluted and appear confusing. Most of them surface concurrently. However, the progression is quite logical and clear if you see them as the body’s way of slowing down, reaching its peak at Phase D of Adrenal Fatigue. Indeed, like a domino effect, the shutting down process happens in steps. At Phase D, the body is reduced to bed rest. Ambulatory help for daily chores are required. Fatigue is extreme with the gastric system paralyzed, heart rate irregular, mental function clearly compromised, while the feeling of wired and tired abounds, as adrenaline is high when energy is low.
The down-regulation or return to simplicity will continue as long as the body sees it as a positive step to conserve energy for survival. As the body further slows down, muscle breaks down to generate energy, leading to an overall net loss of protein and muscle mass. When this happens, the body enters a catabolic state, with overall weight loss and muscle wasting. Fibromyalgia and Chronic Fatigue Syndrome may be triggered. Appetite reduces as the gastrointestinal tract motility slows and gastric capacity reduces. Those with sugar imbalances and insulin resistances are particularly vulnerable to a worsening state. Electrolyte imbalance, especially as it relates to sodium and potassium, becomes common. The myriad of physical symptoms mentioned above is convoluted and appear confusing. Most of them surface concurrently. However, the progression is quite logical and clear if you see them as the body’s way of slowing down, reaching its peak at Phase D of Adrenal Fatigue. Indeed, like a domino effect, the shutting down process happens in steps. At Phase D, the body is reduced to bed rest. Ambulatory help for daily chores are required. Fatigue is extreme with the gastric system paralyzed, heart rate irregular, mental function clearly compromised, while the feeling of wired and tired abounds, as adrenaline is high when energy is low.
This continuum of down-regulation will not stop until the body finds its equilibrium. This is the point where energy demands slow to a point that matches the input. This is the point when the body finally feels it can survive and not threatened. Sad to say many are often bedridden when Adrenal Fatigue reaches this point.
As you can see, low hormonal and low-clearance states, which has began in earlier phases of Adrenal Fatigue, gets worse quickly. These important clinical hallmarks are frequently overlooked.In this phase, the adrenals have lost most of their ability to serve as the body’s stress control center. They become hypersensitive. Attempts to jump-start them quickly usually fail. Traditional medications, nutritional supplementation and the classical macro nutritional programs seldom are successful and may in fact backfire.
 Crashes occur frequently, with delayed recovery. The underlying physiological pathways are not well understood. Conventional scientific logic is unable to solve the puzzle. Looking at the big picture, it is evident that the body’s symptoms are part of an overall process of severe systematic slowing down if not an outright shutting down of internal operations save and except the most essential ones for survival. Conventional medical workup continues to be negative. Functional medicine workup is usually inconclusive. In addition to previously mentioned characteristics of Stage 3C, the following additional unpleasant symptoms commonly surface in this Phase:
Crashes occur frequently, with delayed recovery. The underlying physiological pathways are not well understood. Conventional scientific logic is unable to solve the puzzle. Looking at the big picture, it is evident that the body’s symptoms are part of an overall process of severe systematic slowing down if not an outright shutting down of internal operations save and except the most essential ones for survival. Conventional medical workup continues to be negative. Functional medicine workup is usually inconclusive. In addition to previously mentioned characteristics of Stage 3C, the following additional unpleasant symptoms commonly surface in this Phase:
It is not uncommon to see a reversal of the 24-hour saliva cortisol curve pattern, with low cortisol in the morning and high in the late afternoon and evening. The cortisol to DHEA ratio is generally high. Sufferer is bedridden, unable to do daily chores or walk from room to room without feeling fatigued and drained. Constant ambulatory assistance is required.
Current concepts point to the likelihood of pump failure, receptor site dysfunction, transport system dysregulation, low clearance due to incomplete detoxification, metabolite buildup, Autonomic Nervous System reactive responses, and electron driven retoxification as possible etiology for the wide variety of paradoxical and exaggerated reactions commonly seen in this phase. A key mechanism of this breakdown is by the development of positive feedback loops. The internal self-regulatory loop system of the body is generally based primarily on negative feedback and not on positive feedback circuits. Positive feedback loops are inherently unstable and are usually the cause for the final breakdown in many chronic diseases. For example, failure of the Sympathetic Nervous System (SNS) mentioned earlier causes lightheadedness. There may be a need for prolonged bed rest, which in turn worsens the orthostatic hypotension as the patient tries to get up. Overstimulation of the SNS may lead to rapid heart rate, cardiac arrhythmia, reduced cardiac output, and heart failure. Heart failure will, in turn, trigger more SNS stimulation, and thus propel the viscous cycle downward.
 The timing and rapidity of system failure from the positive feedback loops depend on the dynamic interactions among the various systems in the body, with primary emphasis on the neurological, endocrine, and cardiac systems in an Adrenal Fatigue setting. Breaking the positive feedback loop and allowing the system to reset itself offers the best overall clinical strategy. This can be accomplished with a micro-nutritional approach, foundational and rudimentary diet protocols and medications as needed. Downward titration of micronutrients to match the body’s clearance capacity is the key and if this is done properly, the body’s nutritional needs are attended to without over-burdening the body’s clearance system. The body will slowly become properly nurtured and be given the opportunity to rebuild its own reserve of hormones back to the minimum threshold required for the various organs to function normally.
The timing and rapidity of system failure from the positive feedback loops depend on the dynamic interactions among the various systems in the body, with primary emphasis on the neurological, endocrine, and cardiac systems in an Adrenal Fatigue setting. Breaking the positive feedback loop and allowing the system to reset itself offers the best overall clinical strategy. This can be accomplished with a micro-nutritional approach, foundational and rudimentary diet protocols and medications as needed. Downward titration of micronutrients to match the body’s clearance capacity is the key and if this is done properly, the body’s nutritional needs are attended to without over-burdening the body’s clearance system. The body will slowly become properly nurtured and be given the opportunity to rebuild its own reserve of hormones back to the minimum threshold required for the various organs to function normally.
One common clinical recovery mistake in Phase D is the use of high dose nutrients. Practitioners not well trained in this phase are misled to increase nutritional dosages, thinking that what works before in earlier phases should work better in higher dosages in this phase and as a result, higher doses of Vitamin C, Vitamin B, glandulars, herbs, thyroid support, and glutathione are administered to the patient. Some clinicians may even attempt aggressive toxic metal elimination whilst other practitioners will resort to intravenous delivery systems. Little do they know that high doses may not lead to better results. There may well be a transient period of well-being but these strategies will often fail over time. The body will go through phases of a roller-coaster ride with plateaus, highs, and lows as it tries to restore equilibrium if there is sufficient reserve left to meet the minimum required threshold.Over time, however, the body continues to decompensate as it fails to restore equilibrium with each attempt.While such aggressive nutritional strategy may have worked well in earlier phases and stages of Adrenal Fatigue, the response of high dose nutritional therapy will often become blunted and the overall condition may actually get worse in this phase. Worsening of the patient’s condition upon administration of nutritional supplements or medications is a major hallmark in Adrenal Fatigue Phase D, as evidenced by severe paradoxical reactions associated with a low-clearance state.
To avoid further decompensation, it may be necessary to stop using the high dose nutritional approach temporarily, both at the macro and at the micro levels. Instead, the blueprint of a successful recovery program usually involves a meticulously designed program of micro-nutritionals with dosages timed and titrated downwards to a level acceptable by the patient’s body without creating a toxic retoxification response under a low clearance state. With this approach, the body, over time, will likely assimilate the nutrients properly at a rate it can process comfortably. This will start the stabilization period followed by the rebuilding process. No matter how good the nutrients are forcing nutrients into the body when it is not ready to accept them will only worsen the condition. Using natural unprocessed forms of macronutrients and small doses of micronutrients that are gentle enough to be delivered and affect cellular bioavailability without significant toxic response is a far more effective approach. This may take a few weeks or a few months, depending on the body’s state of function. With the right dosage and proper nutrients, the body will have a chance to stabilize on its own and rebuild, once it is able to “reset” itself. Once significant reserves have been restored to the adrenals, the physician can then revert back to the more aggressive micro-nutritional approach slowly. A macro nutritional approach may gradually be restarted as well. Clinical outcome can be very positive and dramatic. In this phase of Adrenal Fatigue, the key is not to force nutrients into the body when it is weak, but to nurture the adrenals with proper nutrients at a dose the body can process and allow the adrenals to slowly heal themselves.
 Therefore, even basic nutrients that are usually helpful to the adrenal function, such as Vitamin C, B, and others, have to be given very carefully. This is where most self-navigated programs fail. Nutrients, adaptive herbs, or glandulars often behave in a stimulatory fashion in this phase due to the body’s low clearance state. Even steroids or intravenous nutritional delivery may become ineffective and trigger worsening responses. The proper dosage and selection of the right delivery system are critical because cellular bio availablity and metabolic clearance are often severely compromised. Administration of Vitamin C, cortisol, DHEA, and pregnenolone, all of which are normally welcomed by the weak adrenals, cease to bring about any improvement in symptoms but may become ineffective and possibly toxic in this phase of Adrenal Fatigue. In other words, nutrients may back fire and this cannot be overemphasized. The more the adrenals are exhausted, the less they can tolerate medication, nutrients, herbs, or glandulars. It may appear that nothing appears to work and that the brutal downward decompensatory cycle seems to be well entrenched. Sufferers will become desperate and try to overcome their physical and mental exhaustion on their own to no avail. Depression will often set in and suicidal tendencies surface. Physicians are often helpless.
Therefore, even basic nutrients that are usually helpful to the adrenal function, such as Vitamin C, B, and others, have to be given very carefully. This is where most self-navigated programs fail. Nutrients, adaptive herbs, or glandulars often behave in a stimulatory fashion in this phase due to the body’s low clearance state. Even steroids or intravenous nutritional delivery may become ineffective and trigger worsening responses. The proper dosage and selection of the right delivery system are critical because cellular bio availablity and metabolic clearance are often severely compromised. Administration of Vitamin C, cortisol, DHEA, and pregnenolone, all of which are normally welcomed by the weak adrenals, cease to bring about any improvement in symptoms but may become ineffective and possibly toxic in this phase of Adrenal Fatigue. In other words, nutrients may back fire and this cannot be overemphasized. The more the adrenals are exhausted, the less they can tolerate medication, nutrients, herbs, or glandulars. It may appear that nothing appears to work and that the brutal downward decompensatory cycle seems to be well entrenched. Sufferers will become desperate and try to overcome their physical and mental exhaustion on their own to no avail. Depression will often set in and suicidal tendencies surface. Physicians are often helpless.
Progression to this Phase D from earlier phases can be gradual or abrupt. It is not uncommon to see that a stressful event (e.g. death of a loved one, over-exercise, overwork, medication intolerance, excessive exogenous steroid overload from medications, infectious processes such as snake/spider bites or pneumonia) can overwhelm the already decompensated and constitutionally weak adrenals, leading to a rapid descent into Phase D (bypassing earlier phases) within days or weeks.
Phase D Adrenal Fatigue is not a state to be self-navigating. Routine laboratory tests are normally not helpful and may even be confusing at this point. Expert professional guidance is absolutely necessary and if left unattended, the natural progression of Phase D condition will cause further decompensation and ultimate collapse. Unfortunately, qualified physicians in this area are extremely rare. However, recovery is possible and often can be quite speedy and dramatic, but getting the right professional help is the key. A comprehensive recovery program is essential, allowing for some trial and error due to the poorly understood underlying physiology of Adrenal Fatigue.
 The leading reason why Adrenal Fatigue condition has eluded medical investigation for decades is that clinical presentations appear to be non-uniform. The wide variation of possible responses to the same stressor and the resulting level of Adrenal Fatigue often defy medical logic. Some people can be under severe stress and perform well, while others crash when confronted with the slightest stressor. Some Adrenal Fatigue crashes will progress steadily over time, from Stage 1 to Stage 3 slowly, while others jump quickly into Stage 3 and never fully recover.
The leading reason why Adrenal Fatigue condition has eluded medical investigation for decades is that clinical presentations appear to be non-uniform. The wide variation of possible responses to the same stressor and the resulting level of Adrenal Fatigue often defy medical logic. Some people can be under severe stress and perform well, while others crash when confronted with the slightest stressor. Some Adrenal Fatigue crashes will progress steadily over time, from Stage 1 to Stage 3 slowly, while others jump quickly into Stage 3 and never fully recover.
The body’s intrinsic constitution plays a sizable role. The body’s constitution is the body type that you were born with. Some of us have stronger hearts, while others have stronger legs. There are always some weak parts somewhere in our body. Some of us have more, while others have less.
What is apparent in people suffering from Adrenal Fatigue is the body’s ultimate response to stressors depends largely on the body’s intrinsic constitution. Those who have strong adrenal constitutions recover faster and the recovery is sustained when compared to those who have weak adrenals to start with. Oftentimes we see those who have Adrenal Fatigue suffer crashes and never fully recover only to continue going downward in a path of decompensation. There is no laboratory test that can accurately forecast the body’s constitution.Knowing whether you have a strong, normal or weak body constitution plays an important role in adrenal recovery because the pattern of recovery and the kind of nutrients required will differ depending on the type of body constitution. The more advanced the Adrenal Fatigue, the more important the body constitution role in determining the ultimate natural progression of the condition.
The following depicts how the body’s intrinsic adrenal constitution affects the recovery pattern in Stage 3C Adrenal Fatigue:
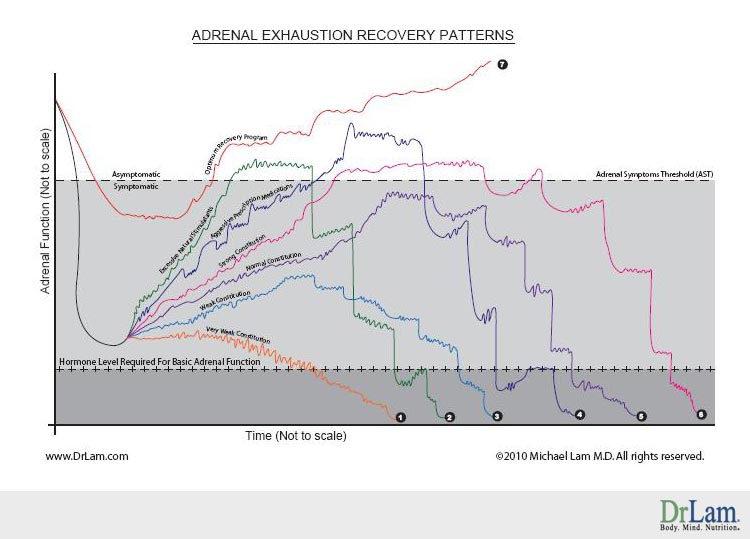
After an adrenal crash, there is no noticeable recovery. The body may go through a period of stabilization, but even this is marred with multiple minor crashes. Severe symptoms continue to persist and they just get worse over time. Not only has recovery failed, but also the energy level continues on a slopping downhill path. From time to time, there will be major crashes that ultimately push the adrenal hormones and functions below the minimum level necessary for normal basic adrenal function. The time frame varies, but this is usually a matter of months, if no attention is given to nurture the adrenals back to health quickly. Any inappropriate use of stimulatory natural compounds or prescription drugs may result in a brief sense of well being at best, but this quickly backfires and makes the situation even worse.
 Those who start out with weak adrenal glands will generally have a mild recovery after a major crash. There may be a sustained period of gradual improvement, but the progress will be very slow. After a while, a plateau is reached, as the energy level of the body cannot be increased any further. When a stressor hits, there will be inevitable follow up crashes, lowering the adrenal function. With each crash, there is a period of stabilization. These periods of stabilization may be accompanied by a slow and gradual reduction in energy level, or at best, maintaining the same energy level. Over a period, of time, the body will likely experience multiple crashes which tend to increase in intensity and severity with longer and longer recovery time. Invariably, the body will be hit with a major crash and enter into Adrenal Fatigue Stage 3D. After a brief pause and declining stabilization period, adrenal failure may ensue.
Those who start out with weak adrenal glands will generally have a mild recovery after a major crash. There may be a sustained period of gradual improvement, but the progress will be very slow. After a while, a plateau is reached, as the energy level of the body cannot be increased any further. When a stressor hits, there will be inevitable follow up crashes, lowering the adrenal function. With each crash, there is a period of stabilization. These periods of stabilization may be accompanied by a slow and gradual reduction in energy level, or at best, maintaining the same energy level. Over a period, of time, the body will likely experience multiple crashes which tend to increase in intensity and severity with longer and longer recovery time. Invariably, the body will be hit with a major crash and enter into Adrenal Fatigue Stage 3D. After a brief pause and declining stabilization period, adrenal failure may ensue.
Those who suffer from Adrenal Exhaustion but have a normal adrenal constitution are likely to be able to mount a reasonable and moderate level of recovery. The recovery pattern is characterized by multiple setbacks and minor crashes along the way, but the setbacks tend to be rhythmic in nature. The body is given some time to adjust. While full recovery is usually not possible, the person remains symptomatic (as the maximum recovery level is below the Adrenal Symptoms Threshold (AST)). Achieving full asymptomatic status is not likely and there is always some discomfort, though the unpleasantness can be reduced with proper rest and lifestyle adjustments. With time however, this is followed by major crashes. With each crash, the body tries to mount a recovery effort. At first, the recovery effort brings relief but over time, as the adrenals get weaker and weaker with continued crashes, the recovery curve tends to be stable at best. Ultimately, the many crashes will be followed by a flat stabilization curve resembling a stair step going down. This process can last for months and even years. Eventually, the body’s reserve is so low that it crashes and enters into Stage 3D Adrenal Fatigue. After a final stabilization period, adrenal failure risk becomes very high.
Those blessed with a strong adrenal constitution usually will be able to mount a significant recovery steadily. The recovery curve is smoother than that of people with a normal constitution. Since the body is stronger, it is able to better absorb the stress and setbacks become less frequent as compared to those in people with normal body constitutions. Eventually, the body is able to return to the level of function above the adrenal threshold level. Sufferers may feel well for a long period of time if this can be sustained. There may be occasional minor crashes but recovery is relatively fast. Eventually, with aging, and if stressors are not removed, a major stress will precipitate a major crash. With time and aging, the crashes become more intense and recovery becomes less successful. Eventually the recovery period is shortened as the body crashes into Adrenal Fatigue Stage 3D and ultimately end in adrenal failure.
 Using natural stimulatory compounds such as certain herbs and glandulars to facilitate Adrenal Exhaustion recovery can be a major mistake, and the following serves to show why. At first, the results are promising and there is usually a fast and furious recovery as the body’s energy level is propped up and sustained.The adrenals are put into overdrive to increase their hormone output and as a result, energy will return to the body. Sometimes, the energy level may even return to that above the adrenal symptoms threshold. While the overall energy level may not be the same as that immediately pre-crash, unpleasant symptoms are at least not prevalent. The sufferer is misled into thinking that his problem has been resolved. The adrenal glands however, have developed a blunted response over time to such continued stimulation strategy. The body’s energy level then plateaus and fails to increase even with increasing doses of natural stimulatory compounds. Eventually, the adrenals will start to fail, and this is usually precipitated by a stressor, triggering a major crash. After the first major crash, more stimulants are usually taken as a follow up. There again may be a period of recovery, but the duration is short, and the level of recovery is mild at best. This is only to be followed by more crashes. With each subsequent crash, the crash intensity is increased. The body’s ability to mount a recovery is blunted, and in fact may slowly decompensate and roll into subsequent crashes, with one crash followed by another. This progression can happen quickly, not far behind those people with the weakest constitution. Those with strong constitutions will do better overall while those with weak constitutions will do significantly worse.
Using natural stimulatory compounds such as certain herbs and glandulars to facilitate Adrenal Exhaustion recovery can be a major mistake, and the following serves to show why. At first, the results are promising and there is usually a fast and furious recovery as the body’s energy level is propped up and sustained.The adrenals are put into overdrive to increase their hormone output and as a result, energy will return to the body. Sometimes, the energy level may even return to that above the adrenal symptoms threshold. While the overall energy level may not be the same as that immediately pre-crash, unpleasant symptoms are at least not prevalent. The sufferer is misled into thinking that his problem has been resolved. The adrenal glands however, have developed a blunted response over time to such continued stimulation strategy. The body’s energy level then plateaus and fails to increase even with increasing doses of natural stimulatory compounds. Eventually, the adrenals will start to fail, and this is usually precipitated by a stressor, triggering a major crash. After the first major crash, more stimulants are usually taken as a follow up. There again may be a period of recovery, but the duration is short, and the level of recovery is mild at best. This is only to be followed by more crashes. With each subsequent crash, the crash intensity is increased. The body’s ability to mount a recovery is blunted, and in fact may slowly decompensate and roll into subsequent crashes, with one crash followed by another. This progression can happen quickly, not far behind those people with the weakest constitution. Those with strong constitutions will do better overall while those with weak constitutions will do significantly worse.
Thyroid and steroid medications are commonly used in Adrenal Fatigue cases during the recovery process . While these potent drugs have their roles to play, aggressive use can make Adrenal Exhaustion cases worse off over time. The most common is thyroid medication that is usually prescribed after the sufferer has visited his physician. Recovery usually tends to be steady and going well at first. With each increase in medication dosage or delivery system, there appears to be a corresponding increase in energy level. The physician is encouraged as his patient’s fatigue condition appears to be getting better and laboratory test results appear to be improving. The sufferer may be asymptomatic as long as his medicine is taken regularly. There may be a peak effect reached when the sufferer feels almost “back to normal.” The only problem is that strong medication is needed to keep this energy level sustained. Over a period of time, steroids may be added as well, with an ever increasing dose. While this may go well for some time, eventually the body will reach its maximum stimulatory level and the adrenals simply cannot be whipped up any more. With the slightest stressors, a major crash will happen. More medication will normally be administered but the patient’s response will be blunted. The crash intensity increases and the recovery effort is marred, followed by more major crashes. Eventually the physician is at a loss what to do next as his major arsenal of drugs is exhausted, only to see his patient’s condition get worse. The sufferer is then abandoned by his physician to self-navigate which often ends disastrously as Adrenal Fatigue Stage 3D. After a brief heroic attempt to reverse failure, adrenal failure risk is usually magnified. Those with strong constitutions will do a bit better overall while those with weak constitutions will do significantly worse.
An optimum recovery program is usually personalized with the use of properly dosed gentle nutrients. This can bypass all the above undesirable patterns (Patterns 1-6) associated with Adrenal Fatigue and its symptoms. By using gentle natural compounds, the body is given the natural tools it needs to heal itself. Crash intensity can be reduced significantly, with a soft landing and minor unpleasantness of symptoms at most. This is followed by a rhythmic recovery back into the asymptomatic zone. Total crash and recovery cycle time will be reduced greatly. There will be provisions made for small setbacks that do not affect normal daily living. As the body reaches the recovery plateau well above the asymptomatic level but not at the pre-crash level, the body is allowed to rest. Using gentle natural compounds that are carefully dosed and delivered to suit the body’s needs, this approach provides a window of opportunity to help build up the body’s reserve and get it ready for the next Recovery Phase. As the body is resetting itself at a higher level of function, the opportunity is there to be seized to propel the body upward toward a higher energy level that is even higher than that of pre-crash. Risk of follow up crashes will therefore become minimal. Those who have weak constitutions will benefit the most from this type of recovery program.
the body is given the natural tools it needs to heal itself. Crash intensity can be reduced significantly, with a soft landing and minor unpleasantness of symptoms at most. This is followed by a rhythmic recovery back into the asymptomatic zone. Total crash and recovery cycle time will be reduced greatly. There will be provisions made for small setbacks that do not affect normal daily living. As the body reaches the recovery plateau well above the asymptomatic level but not at the pre-crash level, the body is allowed to rest. Using gentle natural compounds that are carefully dosed and delivered to suit the body’s needs, this approach provides a window of opportunity to help build up the body’s reserve and get it ready for the next Recovery Phase. As the body is resetting itself at a higher level of function, the opportunity is there to be seized to propel the body upward toward a higher energy level that is even higher than that of pre-crash. Risk of follow up crashes will therefore become minimal. Those who have weak constitutions will benefit the most from this type of recovery program.
The following table summarizes the above discussion:
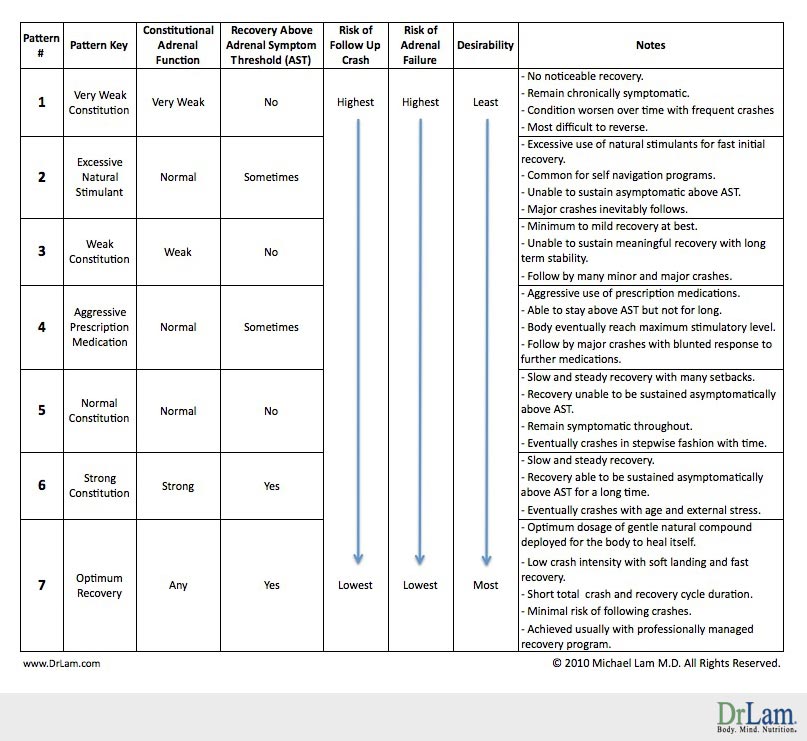
Adrenal Exhaustion recovery patterns vary greatly depending on one’s body constitution and other external factors. The natural progression for those who suffer from normal Adrenal Fatigue is one of slow deterioration over a period of time (Pattern 5). However, the time can be lengthened if the intrinsic body constitution is strong (Pattern 6). The goal is to extend the time as long as possible and the deterioration pattern to be slowed as much as possible. This is best achieved by a personalized recovery program (Pattern 7).
Unfortunately, excessive and inappropriate use of natural stimulatory compounds commonly employed by those who are in self-navigating mode (Pattern 3), as well as the aggressive use of prescription medications (Pattern 4), often make the final outcome of many Adrenal Exhaustion recovery cases worse off. Eventually, this will push the sufferer into adrenal failure far earlier than if nothing is done and nature takes its course (Pattern 5). In other words, matters are often made even worse.
Fortunately, regardless of which recovery pattern is being followed, the body is generally forgiving. The key is to mimic the recovery curve as close as possible to Pattern 7. With the right kind of professional help, the body’s damage can often be reversed and nurtured back to health.
Adrenal Exhaustion refers to Stage 3 of Adrenal Fatigue. In this stage, the body’s ability to function on a day-to-day basis is moderately to severely compromised. This is a nightmare in the making as all organ systems of the body are affected. Without healthy adrenals, virtually no system in the body can work at its optimal state.
Because of total body systemic involvement, Adrenal Exhaustion is associated with a myriad of symptoms that are hard to describe with clarity. Systemic manifestation hypoglycemia, diabetes, chronic pain, fibromyalgia, chronic fatigue, low metabolism, frequent infection, exaggerated auto immune response, hypothyroidism, fluid retention, acute anxiety attack, insomnia, and depression are just some of the disturbing presentations found at this phase of Adrenal Fatigue.
Clinically, Adrenal Exhaustion can broadly be categorized into four overlapping phases that are decidedly indistinct.
In this phase of Adrenal Fatigue, mild symptoms characteristic of first and second stage Adrenal Fatigue continue to worsen and become persistent or chronic. Low blood pressure, fatigue, insomnia, and salt craving are the hallmarks. Sufferers continue to be active physically in self-guided programs or under the care of health care professionals. Numerous doctors are normally consulted by this time, but the condition does not usually improve over time, but in fact, becomes worse.
The endocrine system in our body is linked hormonally in a series of axes for optimal function. The Ovarian-Adrenal-Thyroid axis in women and the Adrenal-Thyroid axis in men are particularly important. Hallmark symptoms include feeling cold, low libido, PMS, irregular menstrual cycles, and sluggishness in addition to the phase A symptoms.
The sufferer’s physical and emotional states continue to deteriorate and he enters into a state of confusion. Most conventional and many naturally oriented physicians alike are at a loss in understanding this phase. Patients are often prescribed anti-depressants and subsequently left to self-navigate through turbulent waters. Not knowing what to do and who to turn to, sufferers continue to self navigate, often using inappropriate nutrients that are not conducive to healing and subjecting their bodies to continued trial and error. This often makes the condition worse off over time.
As the body continues the downward path of impaired function, it gathers steam. The body becomes severely compromised in trying to maintain the fine controls of homeostasis. Normal equilibrium is therefore lost. The body will try its hardest to maintain equilibrium by activating various autonomic and reactive compensatory responses which are the neurological and endocrine systems, but unfortunately, the body’s crude response together with the damaged receptor sites and the impaired metabolic and detoxification pathways give rise to paradoxical and exaggerated responses. The body’s internal thermostat is “broken”. Sufferers are usually frustrated and feel abandoned by their physicians. Hallmark symptoms during this phase of Adrenal Fatigue include heart palpitations, fragile blood pressure, dizziness, lightheadedness, postural hypotension, anxiety attacks and adrenaline rushes. The body is literally “falling apart” internally. Sufferers in this stage are often incapacitated and frequently called the “living dead”. It is imperative people in this phase be taken care of by a qualified specialist physician as this level of dysfunction is well beyond the expertise of even the most astute naturally oriented health care provider.
 As the body’s cortisol level falls below the minimum required for normal daily function and cortisol output fails, the body may down-regulate the amount needed in order to preserve what is on hand for only the most essential of body functions. Positive feedback loop becomes the prominent regulatory circuit. Hallmark symptoms during this phase of Adrenal Fatigue include severe paradoxical reactions and worsening of symptoms with the use of nutritional supplementation and medications. The condition will only get worse if the symptoms are not arrested. This is not a state to be self-navigating in as expert professional guidance is absolutely needed. A carefully planned program of micro-nutritional support and medications will be needed. Unfortunately, qualified physicians in this area are extremely limited.
As the body’s cortisol level falls below the minimum required for normal daily function and cortisol output fails, the body may down-regulate the amount needed in order to preserve what is on hand for only the most essential of body functions. Positive feedback loop becomes the prominent regulatory circuit. Hallmark symptoms during this phase of Adrenal Fatigue include severe paradoxical reactions and worsening of symptoms with the use of nutritional supplementation and medications. The condition will only get worse if the symptoms are not arrested. This is not a state to be self-navigating in as expert professional guidance is absolutely needed. A carefully planned program of micro-nutritional support and medications will be needed. Unfortunately, qualified physicians in this area are extremely limited.
Dissecting through the symptomology and complaints of Adrenal Exhaustion is a daunting task for many health care professionals, except the most astute of physicians trained in this specialized field. The interconnectivity and complexity point to a convoluted picture of conflicting symptoms that defy conventional medicine logic, not because the body behaves illogically, but because our current understanding of adrenal function is still in its infancy. However, recovery can be dramatic and fast if the body is given the right tools to heal itself.
Due to the mind-body systemic involvement in this phase, an integrated approach incorporating fields of neurology, endocrinology, cardiology and psychiatry will be necessary. Attempts to extrapolate our current limited knowledge of single field science into a clinical protocol without consideration of the multi-system involvement often fails and indeed frequently worsens this condition. Navigating through the Adrenal Exhaustion stage should be reserved for only for those health care professionals who are highly knowledgeable and experienced.
You may not have AFS symptoms when you have AFS. There are just so many symptoms that are related to AFS. When you have AFS, you can have an imbalance of your female hormones, which could be the reason why you have miscarriages.
Depending on the stages of AFS you suffer from, exercise needs to be adjusted accordingly. During early stages of Adrenal Fatigue, some aerobic and light weight lifting could be beneficial. But with advanced stages of AFS, even light walking could be a problem.
Light weight strength training would be better. Light walking, biking or swimming is good cardio to do also. It really depend on the severity of your symptoms after you exercise. Start your recovery with rebuilding core strength is the key, and the Adrenal Yoga set of exercises is designed to do this systematically and gently.
It can play a big part over a long period of time.
For those with AFS, autonomic nervous system dysfunction is a common cause