 What is immune nutrition? It’s an approach to planning your diet and supplementation for the best possible immune system benefits. Many conditions could be prevented, reversed, or at least well-managed by improving the immune system. And the immune system’s health is largely based on what kind of nutrition you provide for it. So in this article, we’ll be looking at the three levels of immune nutrition:
What is immune nutrition? It’s an approach to planning your diet and supplementation for the best possible immune system benefits. Many conditions could be prevented, reversed, or at least well-managed by improving the immune system. And the immune system’s health is largely based on what kind of nutrition you provide for it. So in this article, we’ll be looking at the three levels of immune nutrition:
We’ll be talking mostly about these three levels with a focus on immune system health, but bear in mind that they affect all your other organs and systems as well. Your organs and systems exist as a network, and they all affect each other.
Your immune system is divided into two main branches: innate immunity (which is sometimes called natural immunity), and adaptive immunity (which is sometimes called specific immunity). These two branches evolved at different times over millions of years, and innate immunity is the older one.
Innate immunity is broad; it’s a more generalized immune response. It’s very fast-acting, reacting within a few hours but also only lasting a few hours or days. It requires the production and release of a large quantity of immune cells. That’s because it’s not specific, it doesn’t have a memory of what threats your body has been exposed to before, unlike adaptive immunity.
Innate immunity utilizes phagocytes, which are immune cells that engulf the threat. Some examples of phagocytes are neutrophils and macrophages. Both of these are white blood cells. It also utilizes natural killer cells (NKs), whose job is to kill the cells in your body that are abnormal, like cancer cells, or have been infected or damaged by a pathogen or toxin. Cytokines are the messengers of your innate immunity. They tell it where the invasion or injury is so that it can direct its phagocytes or NKs there.
The newer branch of your immune system is adaptive immunity. It evolved to fill the gap that innate immunity leaves – that of not having a memory. When a pathogen enters your body and your adaptive immunity is exposed to it, it will keep a memory of it. It takes longer to respond, in the order of a few days. But the memory lasts a long time, sometimes for decades, so you become immune to certain pathogens for that duration.
Adaptive immune cells are mainly lymphocytes – B cells and T cells. These two types of cells function in different zones of your body. B cells proliferate through your lymphatic system, which is why this part of your immune system is sometimes called humoral immunity. T cells function within cells, and they target viruses and tumors by creating cytokines. This part of your immune system is sometimes called cellular immunity or cell-mediated immunity.
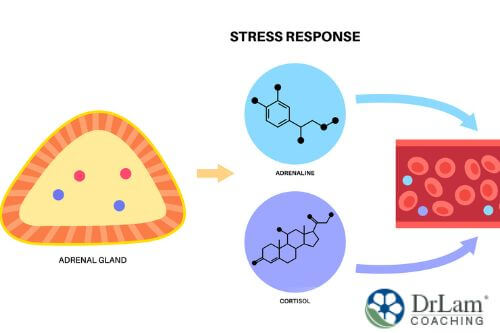 The NeuroEndoMetabolic (NEM) Stress Response is your body’s global response to stress. It goes beyond the adrenal glands and utilizes a network of organs and systems to fight stress. It’s composed of six circuits: the Hormone, the Bioenergetics, the Cardionomic, the Neuroaffect, the Inflammation, and the Detoxification circuits. The adrenal glands are part of the Hormone and Cardionomic circuits, and they are the NEM’s first responders.
The NeuroEndoMetabolic (NEM) Stress Response is your body’s global response to stress. It goes beyond the adrenal glands and utilizes a network of organs and systems to fight stress. It’s composed of six circuits: the Hormone, the Bioenergetics, the Cardionomic, the Neuroaffect, the Inflammation, and the Detoxification circuits. The adrenal glands are part of the Hormone and Cardionomic circuits, and they are the NEM’s first responders.
When it comes to the immune system, the Inflammation Circuit is the most pertinent. It’s composed of the immune system, the gastrointestinal (GI) tract, and the microbiome. The immune system is also a component of your Detoxification Circuit, along with the liver and interstitium. Inflammation and detoxification work hand in hand to help neutralize and get rid of pathogens, toxins, and dead and damaged cells.
As you can see, your immune system is a complex and intelligent system. It has to be aware of what’s going on inside your body as well as with the environment. It is always learning and adapting in what we can call a homeodynamic way. But it can also be overwhelmed by the amount of pressure it's exposed to, including, but not limited to, the following:
To illustrate how food can negatively affect your immunity, let’s take a look at what happens if you’re constantly consuming a food that you’re sensitive to.
The relationship between your immune system and GI tract goes beyond the nutrients that your food provides for your immune cells. In fact, two-thirds of your immune cells are located in your gut in what’s called the gut-associated lymphoid tissue (GALT). The GALT is the main reason why most inflammation begins in the gut.
When you eat foods you’re sensitive to, it can lead to gut dysbiosis. Dysbiosis is when your microbiome becomes imbalanced. This can increase the permeability of your gut lining, allowing substances into your bloodstream that shouldn’t be there. Of course, your immune system flags those as threats and attacks them, causing inflammation there.
Interestingly, there are food sensitivities that don’t always manifest as GI tract symptoms. So you might not make the connection that they are causing whatever other symptoms you’re experiencing. For example, gluten sensitivity can result in neuropsychiatric symptoms that you then think are due to some mental health issues. You might get treated for those mental health issues but keep eating gluten, so the cycle continues. Your immune system is constantly switched on, creating chronic inflammation.
That’s why immune nutrition isn’t just about what you put into your diet, but also about what you take out. We sometimes recommend an elimination diet as a possible solution to this, although our adrenal fatigue diet is already free of the most common irritating and allergenic foods.
 Nutrition is definitely one of the biggest, if not the biggest, factors that affect how well your immune system functions. But there are a few other factors that play a role as well, and it’s important for you to understand them as, if you’re really lacking in one area, immune nutrition will only go so far.
Nutrition is definitely one of the biggest, if not the biggest, factors that affect how well your immune system functions. But there are a few other factors that play a role as well, and it’s important for you to understand them as, if you’re really lacking in one area, immune nutrition will only go so far.
Other than nutrition, sleep is possibly the most influential factor when it comes to immune health as well as overall health. More and more research is coming out confirming how big of an influence it really is. Just a couple of days of interrupted sleep and your physical and mental health can take a dip.
And, if you have a condition that makes it difficult to get good quality sleep, like adrenal fatigue, the bad sleep will worsen it and make it more difficult to recover from it. It will also make you more susceptible to other conditions as well. So getting your sleep right is a huge priority, and for most people, all it takes is creating a solid and sustainable sleep hygiene routine.
Although some stress is unavoidable, and some types of stress are actually healthy and necessary, chronic stress is a huge problem. And it is a root cause for many chronic conditions, including Adrenal Fatigue Syndrome (AFS). With chronic stress, your adrenal glands have to overwork to produce more and more cortisol, your body’s main anti-stress hormone. Eventually, they will become exhausted and their cortisol output will drop.
Both of these situations are part of the progression of AFS, as too high or too low cortisol levels will bring about AFS symptoms. Symptoms of AFS include fatigue, weight gain, sleep disturbances, brain fog, anxiety, mild depression, hair loss, dry skin, loss of libido, estrogen dominance, PMS, infertility, food and drug sensitivities, unstable blood pressure, hypoglycemia, salt and sugar cravings, and lowered immunity.
When you’re suffering from AFS or chronic stress, you’re much more susceptible to recurring infections, including frequent colds and flu. Also, you may be more susceptible to having worse symptoms from these infections, including from COVID-19. That’s why chronic stress can be such a vicious cycle, because it gets you sick, which then makes you more stressed out, so on and so forth. So it is vital you get your stress levels under control.
There is a loneliness epidemic around the world. And even though we’re more connected online than ever before, these types of connections don’t replace the face-to-face kind. Some people say it makes their loneliness even worse. Add to that a few years of lockdowns and quarantines, and this issue has grown exponentially.
 Human beings are deeply social creatures. We cannot survive without some kind of connection. And the lack of connection can lead to not only mental health issues, but to physical health problems as well. Babies deprived of physical touch can die, even if they are fed. And although there needs to be a structural change to the way our societies are set up in order to prioritize community and belonging more, you will have to find your own way to connect for the time being.
Human beings are deeply social creatures. We cannot survive without some kind of connection. And the lack of connection can lead to not only mental health issues, but to physical health problems as well. Babies deprived of physical touch can die, even if they are fed. And although there needs to be a structural change to the way our societies are set up in order to prioritize community and belonging more, you will have to find your own way to connect for the time being.
A sedentary lifestyle is bad for your health, mental clarity, emotional wellbeing, and immune function. Being physically active is the natural state of the human body. We’re not meant to sit at a desk all day and then flop down on the couch for the rest of the night. But, with the way things are, it may be that you have to schedule time for exercise or activity. And that’s fine; it’s a good solution.
An important precaution: if you have AFS or some other debilitating health condition, physical exertion may make it worse. In such cases, it’s better to do very gentle forms of exercise, like adrenal breathing or adrenal yoga. Once you’re well on your way to recovery, you can begin to intensify your exercises gradually.
Once you've considered ways to support your immune health through your lifestyle, you're ready to get into the details of how to make sure your diet supports your immune system as well.
There are two important points to consider when looking at your diet’s macronutrient composition. The first is the type of carbohydrates you consume, and the second is the amount of fiber you consume.
Generally speaking, we recommend that most, if not all, of your meals contain healthy sources of proteins, fats, and fiber. That combination is good for satiety, blood sugar control, gut health, bowel movements, and for repairing and building your muscles and tissues.
The types of carbohydrates you eat affect your glucose metabolism. Carbohydrates are converted into glucose during digestion, and that glucose is released into your bloodstream. There, insulin will pick it up and carry it to your cells where it will be used by the mitochondria for energy production. But not all carbohydrates are equal.
Some carbs will be quickly digested and then release their glucose all of a sudden, spiking your blood sugar levels and causing a state of hyperglycemia. Hyperglycemia, especially if it’s chronic, is very dangerous to health. It’s what people with diabetes have to control on a daily basis. But hyperglycemia can lead to hypoglycemia, or low blood sugar, which is also quite dangerous. What happens is that when there’s a sudden spike in blood sugar levels, your pancreas secretes a lot of insulin, also all of a sudden, to deal with it. This flood of insulin will cause your blood sugar to crash. That's hypoglycemia, and it will prompt you to crave sweets in order to raise your blood sugar levels again.
This cycle is extremely stressful on the body. Panic can also come with hypoglycemic episodes. It manifests as anxiety, shakiness, lightheadedness, brain fog, extreme hunger, and rapid heart rate, to name a few. This cycle will also increase the production of inflammatory cytokines.
 One very effective way to interrupt a cycle like this is to switch to whole grains and complex carbohydrates. These are digested more slowly, so they release their glucose more gradually. This means your pancreas doesn’t have to suddenly increase its insulin secretion, and you don’t get spikes or crashes anymore. Another way is to pair your carbs with fats and proteins, which also slow down the speed of their digestion.
One very effective way to interrupt a cycle like this is to switch to whole grains and complex carbohydrates. These are digested more slowly, so they release their glucose more gradually. This means your pancreas doesn’t have to suddenly increase its insulin secretion, and you don’t get spikes or crashes anymore. Another way is to pair your carbs with fats and proteins, which also slow down the speed of their digestion.
It's also a good idea to learn about glycemic load and glycemic index. Those are scales that can help you figure out how much and how fast a carbohydrate-rich food, including fruits, will release glucose. Foods high on these scales tend to raise blood sugar levels quite quickly, while foods low on them will help stabilize your blood sugar levels. High glycemic index foods are also associated with higher inflammation levels.
Unstable blood sugar levels can weaken your adrenals because they are a big stressor on the body. They will make your NEM overwork, especially if it’s a chronic issue. Diabetics, for example, generally have lowered immunity. And type 1 diabetes is an autoimmune disorder, where the immune system has attacked the pancreatic b-cells that produce insulin. So there is a strong link between glucose metabolism and immunity, and we urge you to be aware of it.
One of the biggest benefits of increasing your fiber intake is how it will affect gut health. Remember how the GALT makes up two-thirds of your immune system cells? It is why having a healthy gut and microbiome is essential for a healthy immune system. And fiber is a cornerstone of gut health.
There are two types of fiber, both of which have their own benefits – soluble and insoluble fiber. Soluble fiber feeds your gut’s good bacteria, so is important for microbiome balance. It also helps slow the release of glucose, lowers cholesterol, reduces fat absorption, and is great for heart health. Insoluble fiber helps with gut motility and cleaning out your GI tract.
Most people are not getting enough fiber. Try to aim for 28-35 grams a day, and from different sources. Fruits and vegetables as well as whole grains are good options. Other ways to improve your gut health and your gut’s microbiome is to eat fermented foods like kefir, yogurt, sauerkraut, and kimchi. You may also want to consider supplementing with a good probiotic, but only if your healthcare professional recommends it.
When it comes to protein, there is a correlation between low protein status and an increased risk of infection. That may be due to how low protein leads to less immunoglobulin production and also a less healthy GALT. The source of dietary protein is important, as you need to get the full range of amino acids. Cysteine helps with glutathione production and glutathione is a powerful antioxidant. Glutamine helps with healing the gut as well as providing energy for your immune cells.
 You should avoid eating too much animal protein because of how it is inflammatory. Dairy and processed meat tend to be the most inflammatory. You can opt for wild-caught fish as a better option, as well as some plant-based proteins like beans and lentils.
You should avoid eating too much animal protein because of how it is inflammatory. Dairy and processed meat tend to be the most inflammatory. You can opt for wild-caught fish as a better option, as well as some plant-based proteins like beans and lentils.
When it comes to fats, it’s all about the kind of fat you consume. Trans fat is very inflammatory, especially when it’s synthetically produced, like in margarine and partially hydrogenated oils. Saturated fats are also inflammatory, though not as much. The healthiest fats are unsaturated and polyunsaturated fat. Also, aim to balance the omega-3 to omega-6 ratio. Most people are overdoing it with omega-6 and not getting enough omega-3 fatty acids.
Even certain healthy fats, like olive oil, can become inflammatory depending on their use. Cooking with oil is not the healthiest, especially on high heat. Better to steam or bake your food and then add the oil at the end.
The following is a list of the most important micronutrients, including vitamins and minerals, for a healthy immune system. Sometimes it is difficult to get all of them through your diet, especially if you’re just starting out with healthy eating. So there is the option of supplementing as well. But with supplements, you need to be careful, especially if you have AFS. AFS increases your risk for paradoxical reactions and even adrenal crashes. Consulting an experienced healthcare professional before taking any supplements will save you a lot of trouble.
Vitamin A is important for the epithelium, the innate immune cells, and the mucosal layers. Its deficiency is most common in pregnant women, children, and people with certain conditions. Vitamin A deficiency increases the risk of infections. You can get dietary vitamin A in the form of carotenoids from fruits like peaches, apricots, mangoes, cantaloupes, and papayas, and from vegetables like yams, broccoli, pumpkins, carrots, and spinach. Vitamin A in the form of retinol is found in oily fish, eggs, milk, and cheese.
B vitamins, including B1, B2, B3, B6, B9, and B12 are important for energy metabolism, lowering inflammation, and fighting free radicals. Each one has its own role in immune nutrition, and a deficiency in each one will cause a slightly different problem. B12 deficiency is a risk for those eating a plant-based diet and should be supplemented. Rich sources of dietary B vitamins include nuts, seeds, leafy greens, whole grains, legumes, and organ meats.
Vitamin B5, which is also called pantothenic acid, along with its metabolically active form pantethine, are important in adrenal fatigue recovery. They are converted to coenzyme A, which helps break down protein, fats, and carbs into energy. Energy is quite depleted in AFS, so anything that helps increase its production can be useful. But coenzyme A also helps in the synthesis of cholesterol, which is the precursor to many adrenal hormones.
 Of course, we can’t talk about immune nutrition without mentioning vitamin C, the most well-established immune-system-supporting vitamin along with vitamin D. Vitamin C is also an anti-histamine and an antioxidant. It helps with the synthesis of collagen, neurotransmitters, and L-carnitine, as well as with the absorption of iron.
Of course, we can’t talk about immune nutrition without mentioning vitamin C, the most well-established immune-system-supporting vitamin along with vitamin D. Vitamin C is also an anti-histamine and an antioxidant. It helps with the synthesis of collagen, neurotransmitters, and L-carnitine, as well as with the absorption of iron.
More specific to the immune system, vitamin C supports the differentiation and maturation of T-cells and NK cells and lowers inflammation. It also helps detoxify the body from dead and damaged macrophages and neutrophils. Many fruits and vegetables contain enough vitamin C for those without a deficiency.
Subclinical vitamin C deficiency is also one of the most prevalent deficiencies in AFS. Along with the brain, the adrenal glands actually have the body’s highest concentrations of vitamin C. That’s why a deficiency results in lower adrenal function and cortisol production. It’s one of the supplements we recommend to our clients the most when undergoing adrenal fatigue recovery. Usually between 200 and 2000 mg per day.
Each client that comes to us will have different needs and goals. So we personalize our nutrition and supplementation plans to fit those differences. If you’d like to learn more about our whole-person approach, including immune nutrition, you can call us for a free initial consultation and talk to one of our expert coaches.
Another immune nutrition superstar is vitamin D. Vitamin D is more like a hormone than a vitamin, and it's produced in your skin upon exposure to sunlight. It is vital for the regulation of your entire immune response, from inflammation, to innate immunity, to adaptive immunity. Food sources of vitamin D include mushrooms, seafood, and eggs. Most people should be supplementing, however, since the best source is sunlight, and sun exposure has been linked to higher cancer risk and skin aging.
Iron is another common deficiency, and this deficiency is associated with respiratory infections, lower T-cell production, and anemia. It is more common in those that consume less meat. At the same time, there is a risk of overdoing it with iron and causing oxidative stress. This is another reason why supplementation is something to do only under the guidance of a healthcare professional that understands your entire health picture. Food sources of iron include fortified grains, organ meats, beef, legumes, dark chocolate, and green leafy vegetables.
Magnesium deficiency is common due to the depletion of our soil, with almost two-thirds of the US population deficient. Aging and certain medications also reduce its absorption. There are different forms of it, such as magnesium oxide, magnesium citrate, and magnesium glycinate. Magnesium oxide is not as well-absorbed as the others, so if you will be supplementing, it’s good to keep that in mind. 350 mg per day is a tolerable dose, although we do sometimes give higher doses to certain clients.
Magnesium and vitamin D are intricately linked. Magnesium is a required cofactor for vitamin D activation, while vitamin D deficiency reduces your gut’s absorption of magnesium. Food sources of magnesium include nuts, seeds, legumes, and greens.
 Zinc deficiency is associated with an increase in the risk of pneumonia and viral infections. It’s also been implicated in COVID-19 infections. It’s common in the elderly, vegans and vegetarians, those who consume alcohol more frequently, and those with chronic conditions.
Zinc deficiency is associated with an increase in the risk of pneumonia and viral infections. It’s also been implicated in COVID-19 infections. It’s common in the elderly, vegans and vegetarians, those who consume alcohol more frequently, and those with chronic conditions.
Zinc is important for the integrity of your mucus membrane, your skin, immune cell growth, and the release of cytokines. Food sources of zinc include beef, turkey, seafood, lamb, eggs, nuts, seeds, yogurt, and legumes. Aim for 8-11 mg per day.
Fruits, vegetables, and herbs are rich sources of different vitamins and minerals. But they also contain phytonutrients. These are plant compounds that have specific immune nutrition effects. Phytonutrients are responsible for the colors of the plants, and those colors can help inform you of their benefits.
For example:
Red, purple, and blue fruits and vegetables have the highest antioxidant concentration. Many plants contain a combination of different phytonutrients. There are, however, certain compounds in plants that some dub as anti-nutrients. These include lectins, oxalates, tannins, phytates, and phytoestrogens. The research is still mixed on this topic, although it seems that it’s only certain individuals, such as those with autoimmune conditions, that may be vulnerable to their negative effects.
Finally, we’d like to briefly mention the benefits of cooking with spices. Many spices have anti-inflammatory, blood sugar-stabilizing, digestion-improving, anti-viral/anti-bacterial, and immune-supporting effects. Some spices to consider including in your cooking are turmeric, ginger, cinnamon, cloves, rosemary, and mint. There are many others.
Immune nutrition is a lifestyle. It has to do with planning your meals around nutrient-dense, anti-inflammatory, gut-healing, and immune-supporting foods. There are three levels of immune nutrition to consider, and they are the macronutrient, micronutrient, and phytonutrient content of the foods you’re eating. Each level should be adjusted to help give you the biggest immune-boosting benefits possible
Some of the most important steps you can take are to stabilize your blood sugar levels by eating foods that are lower on the glycemic index scale, upping your fiber intake, and eating the rainbow to ensure a wide array of micronutrient and phytonutrient consumption.
If you have deficiencies or nutritional gaps, or if you need a boost, you may consider supplementing. But this is something you have to do under supervision, especially if you have AFS or NEM dysregulation. If you’d like to talk to one of our coaches about your options, you can call us for a free initial consultation. We’d be happy to talk to you.
Immune nutrition is all about eating for the health and strength of your immune system. And there are three levels to consider: the macronutrient, micronutrient, and phytonutrient content of your diet. It also depends on your current condition, goals, needs, and some lifestyle factors as well.